The story of the damage that patient support groups allegedly do is intriguing. SW was obviously a keen proponent of the idea. It is , I think, unclear who originated it.
One of the things I've looked into. At this point I'd say the originator is Wessely (though this topic is a process in development and I'm currently looking at other things) with Sharpe giving it a place in the CBM.
In January 1989, in the first article where he is proposing "treating" ME patients with CBT, he is actually published as saying: "Self-help groups can provide considerable emotional and practical support..[...].. Self-help manuals are also useful, and an informative handout should accompany the initial interview."
He means of course stuff he approves of, like stuff from Richard Edwards and a terrible book with a cover blurb promising to bring back the "spark" in the life of 'fatigued women', but the general idea is: support and info are good.
Butler and Chalder, his collaborators who provide him with the CBT expertise, even write an article for MEA, that is published in the Summer 1989 MEA Newsletter. (With thanks to
@chrisb for providing that information.)
But from there things seem to sour.*
One of the things that happens is that there are a couple of books published in 1989 by people associated with ME support groups; D. Smith and C. Sheperd from the ME Association, and M. Franklin and A. MacIntyre from the ME Action Campaign.
Wessely obviously feels very attacked by them and writes a long, very vitriolic piece about them in his buddy journal (BMJ, 3rd June 1989
What your patient may be reading), where he portrays them as a sort of fiction and complains about how "especially psychiatrists" are "the villains", ending with "a little more psychology and a little less T cells would be wellcome".
Basically the ME-organisations are not particularly cheerleading his theories about ME and the accompanying CBT approach, although, looking back, they are actually quite open to some of the underlying theories and CBT as a serious treatment option. (There are of course also pieces that are very critical, like a response to Butler and Chalder's MEA piece with a bunch of scientific articles referenced - they will not have liked their patients having access to that.)
From this point on Wessely is homing in on patient's so-called "hostility" towards psychiatry.
*He could of course very well privately have had those ideas before, with the positive support group remark just him opportunistically saying what he thought landed best at his audience, posing as a benevolent ME patient helper, but I do get the impression it is like the angry response of a toxic boy who had expected to be greeted by his targeted girl with open arms, admiration and gratitude for his perceived awesomeness, and then wasn't.
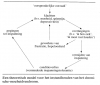
In April 1989 Sharpe, who is in contact with Wessely, also starts to complain about the ME Association and the ME Action Campaign, because they are "rather disparaging of psychiatric treatment", advising that patients need to be encouraged to be as sceptical to their advice as they are about psychiatric treatments. He is at this point for me the first one that explicitly fits those support groups in the CBM, in a way that his Psych Department developed at the time, by assigning them to being a "maintaining factor".
While the notion of ME support groups being harmful to patients fits perfectly with the notions around hysteria, which were the basis for Wessely's image of ME (so I think the general idea is his), it was as far as I can tell so far Sharpe&co who first explicitly fit it into the illness model.
ps: thanks for bringing it up Chris, as because of it I found a possibly important snippet of information in one of my papers.