You are using an out of date browser. It may not display this or other websites correctly.
You should upgrade or use an alternative browser.
You should upgrade or use an alternative browser.
News about Long Covid including its relationship to ME/CFS 2020 to 2021
- Thread starter Hip
- Start date
- Status
- Not open for further replies.
Arnie Pye
Senior Member (Voting Rights)
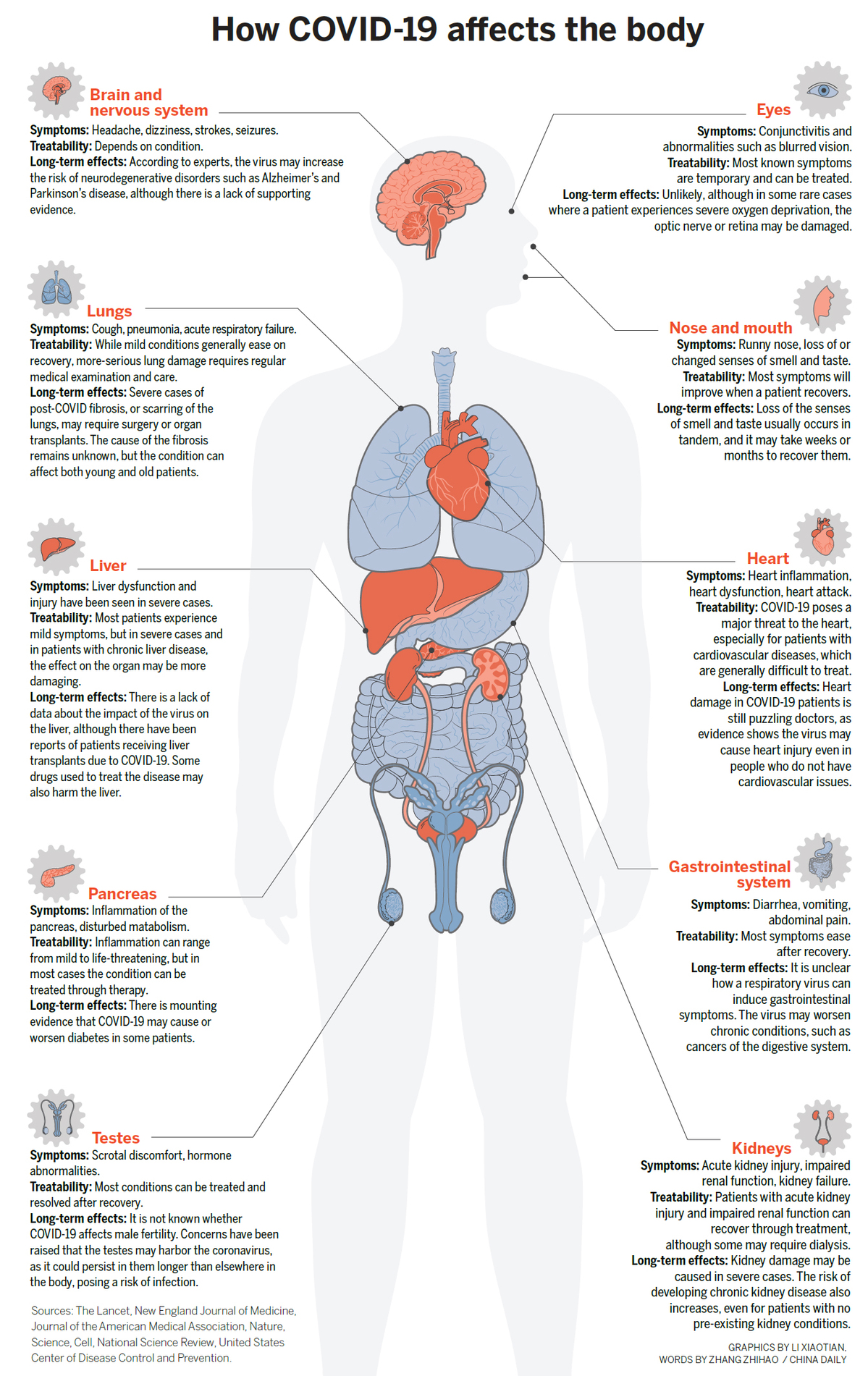
Summary of how Covid affects the body in the short and long term.
Source : https://www.chinadaily.com.cn/a/202007/31/WS5f237414a31083481725d51f.html
Edit : I've just noticed that men are covered by this picture, but women aren't. In other words, the testes and male fertility get a mention but ovaries and female fertility don't.
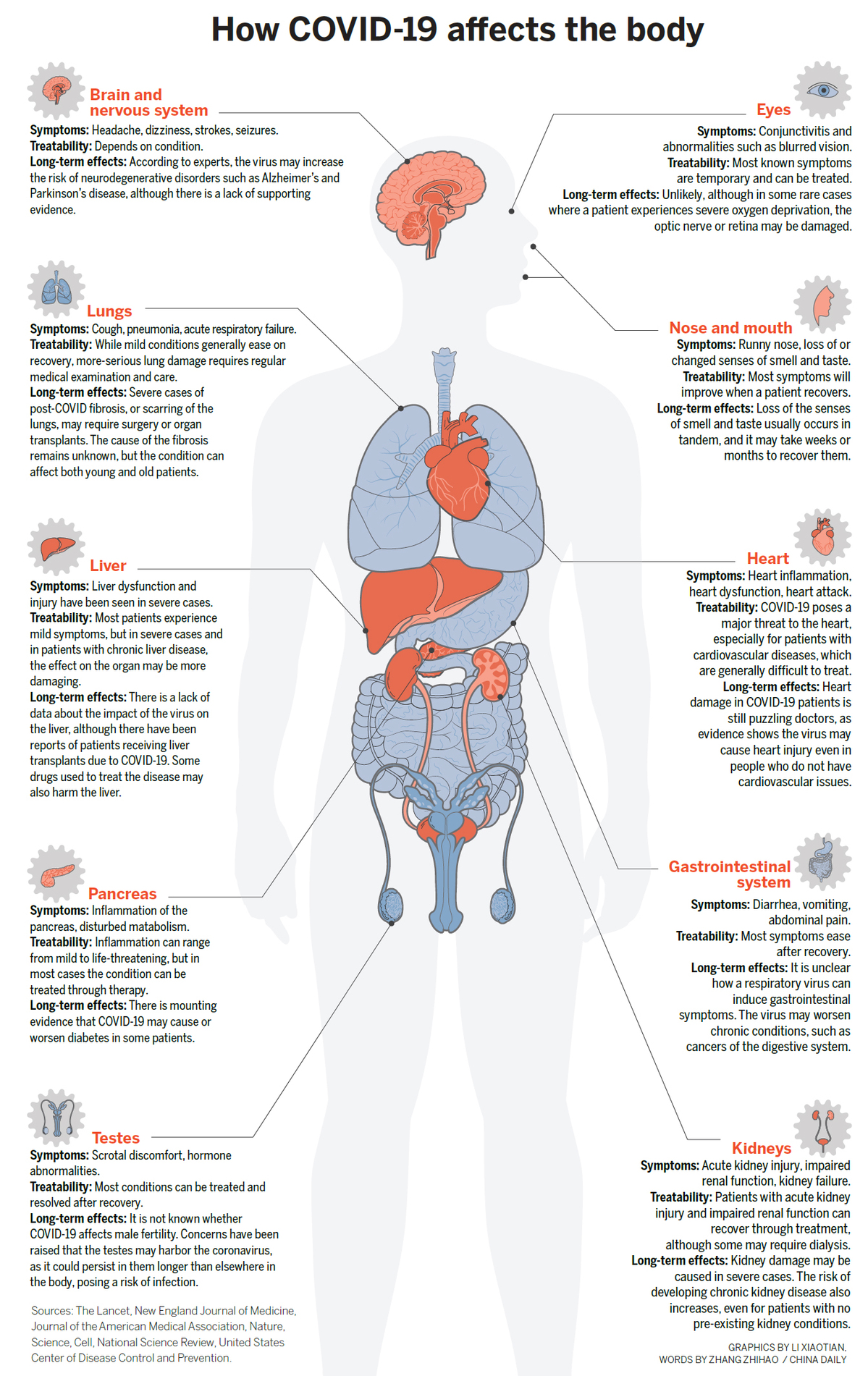
Source : https://www.chinadaily.com.cn/a/202007/31/WS5f237414a31083481725d51f.html
Edit : I've just noticed that men are covered by this picture, but women aren't. In other words, the testes and male fertility get a mention but ovaries and female fertility don't.
Invisible Woman
Senior Member (Voting Rights)
Pray what are these "specialist clinics were genuinely excellent" dispensing and has it been validated [and not by GRADE]?
Or is it just the fine Doctors who lead them?
Well, it probably isn't the patients' opinion if the CFS clinics are anything to go by. As many of them.don't think it's possible for patients to be harmed by their treatments they don't record harms or outcomes.
Jonathan Edwards
Senior Member (Voting Rights)
People are debating with Rachel Pope on Twitter. I'm inclined to ignore her here and let the Twittersphere sort her out! She's not a medical doctor, and is just expressing a personal opinion.
And a right muddle it is too.
rvallee
Senior Member (Voting Rights)
Yeah, same, just saw what you probably mean and yikes (and if not the same then double yikes). Ignore and/or block. Some people are just naturally unpleasant.Upgraded to a block. Her attitude to someone who tried to discuss the matter with her was appalling.
Sly Saint
Senior Member (Voting Rights)
just came across this video on Youtube;
woman with ME who I'm guessing (from her description of what she is normally able to do) might be 'classified' as 'mild', but has had a relapse.
see around 9.00 where she says she gets chest pains, breathlessness.
Maybe a good example for Dr Pope and other LC who dismiss possibility of ME.
woman with ME who I'm guessing (from her description of what she is normally able to do) might be 'classified' as 'mild', but has had a relapse.
see around 9.00 where she says she gets chest pains, breathlessness.
Maybe a good example for Dr Pope and other LC who dismiss possibility of ME.
Code:
https://www.youtube.com/watch?v=3O7_2u9Ng6kSly Saint
Senior Member (Voting Rights)
nbcnews.com
Opinion | Women are more likely to be Covid long-haulers. Here's why that matters.
Opinion | Women are more likely to be Covid long-haulers. Here's why that matters.
While more men have died of Covid-19 at time of writing, Frances Williams, a professor of genomic epidemiology at King's College London, says that preliminary data from the Covid Symptom Tracker app — which she helped develop — shows women are slightly more likely to suffer long-term effects following a Covid infection.
By way of contrast, in post-viral fatigue, women outnumber men two to one. In chronic fatigue syndrome (or myalgic encephalomyelitis), they make up 85 percent of patients.
https://www.nbcnews.com/think/opini...re-often-women-maybe-it-ll-change-ncna1259686Early data coming from online Covid support groups certainly seems to mirror this — although this could change with time. This cohort appears to consist of patients who are relatively young and previously healthy, which is also the case with people who acquire CFS/ME.
As I have documented in "Pain and Prejudice: How the Medical System Ignores Women — and What We Can Do About It," CFS/ME is one of 10 overlapping chronic pain conditions that predominantly affect women; all suffer from stigmatization, lack of research and poor treatment offerings.
mango
Senior Member (Voting Rights)
From the News from Scandinavia thread, about ME and long covid on the Swedish morning tv show Malou Efter Tio:
Watch a part of the interview with Björn Bragée here:
https://www.tv4.se/artikel/71qQqKd4...tidscovid-samma-som-me-bjoern-bragee-reder-ut
Google Translate said:Is long-term covid the same as ME? - Björn Bragée clarifies
"Same symptoms - medically it is similar"
The other day, a column was spread by journalist Agnes Arpi in which she writes about the similarities between ME and long-term covid and she describes Sweden as newly awakened and muddle-headed in this matter. Patients are diagnosed with "anxiety" in their medical records and are forced to return to work even though they feel very bad and have lots of strange symptoms.
Is there something in Agnes Arpi's worries? Is long-term covid the same as ME? Björn Bragée, pain doctor at Bragée clinics and expert at ME, tells what the research says.
ETA: Agnes Arpi is also interviewed in the long covid video.
Kalliope
Senior Member (Voting Rights)
Overall a good article, but apparently the author didn't read Paul Garner's most recent BMJ blog post..nbcnews.com
Opinion | Women are more likely to be Covid long-haulers. Here's why that matters.
https://www.nbcnews.com/think/opini...re-often-women-maybe-it-ll-change-ncna1259686
Kalliope
Senior Member (Voting Rights)
The Atlantic: Unlocking the Mysteries of Long COVID by Meghan O'Rourke
Quotes where ME is mentioned:
- The patients’ symptoms were too varied to be lumped under an established label; in some ways the condition resembled dysautonomia, and POTS in particular—but it was not textbook. (Some clinicians began calling it post-COVID POTS.) In other ways, it closely resembled myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS), in which people alsodemonstrate exercise intolerance and profound fatigue, but it was likewise not textbook. Same for autoimmune disorders. A commonality stood out: These are all poorly understood conditions that, evidence suggests, can be triggered by the body’s response to infections, with clusters of system-roaming symptoms that get grouped under one name.
...
- IF THERE IS any reason for hope in the growing epidemic of long COVID, it is that some academic medical centers are taking these patients seriously and tailoring treatment to them. Medicine’s history with hard-to-identify chronic illnesses, particularly those that mainly affect women, has not been a good one. For decades now, marginalized patients who have felt mysteriously unwell—with ME/CFS, with post-treatment Lyme disease syndrome, with Ehlers-Danlos syndrome, and more—have banded together into activist groups to try to legitimize their suffering. The same is happening online in the long-hauler groups, which are full of patients who have been met with disbelief by local physicians. But the Mount Sinai doctors (along with collaborative teams in various other academic centers) have responded promptly to the problem. Recently, the NIH and the World Health Organization recognized long COVID as a syndrome that warrants more research.
...
- Doing better by these patients has been challenging because 20th-century medicine was not really built to treat hard-to-measure systemic illnesses—especially those, like dysautonomia, ME/CFS, and autoimmune diseases, that can be worsened by stress. Instead, it was based on the rather incredible notion that all bodies respond roughly the same way to infection or injury, and the immune system is a well-organized defense mechanism that never attacks the body. This perspective is turning out to be oversimplified.
...
- “I wouldn’t be surprised if people are walking about with long Epstein-Barr virus, or long influenza. We all know someone who is low energy, who’s told to work harder. We have all heard about chronic-Lyme sufferers, and those with ME/CFS. But they get written off,” Spencer told me. The difference now is that it is happening “on such a huge scale—unlike anything we’ve seen before. It is harder for the medical community to write off.”
Quotes where ME is mentioned:
- The patients’ symptoms were too varied to be lumped under an established label; in some ways the condition resembled dysautonomia, and POTS in particular—but it was not textbook. (Some clinicians began calling it post-COVID POTS.) In other ways, it closely resembled myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS), in which people alsodemonstrate exercise intolerance and profound fatigue, but it was likewise not textbook. Same for autoimmune disorders. A commonality stood out: These are all poorly understood conditions that, evidence suggests, can be triggered by the body’s response to infections, with clusters of system-roaming symptoms that get grouped under one name.
...
- IF THERE IS any reason for hope in the growing epidemic of long COVID, it is that some academic medical centers are taking these patients seriously and tailoring treatment to them. Medicine’s history with hard-to-identify chronic illnesses, particularly those that mainly affect women, has not been a good one. For decades now, marginalized patients who have felt mysteriously unwell—with ME/CFS, with post-treatment Lyme disease syndrome, with Ehlers-Danlos syndrome, and more—have banded together into activist groups to try to legitimize their suffering. The same is happening online in the long-hauler groups, which are full of patients who have been met with disbelief by local physicians. But the Mount Sinai doctors (along with collaborative teams in various other academic centers) have responded promptly to the problem. Recently, the NIH and the World Health Organization recognized long COVID as a syndrome that warrants more research.
...
- Doing better by these patients has been challenging because 20th-century medicine was not really built to treat hard-to-measure systemic illnesses—especially those, like dysautonomia, ME/CFS, and autoimmune diseases, that can be worsened by stress. Instead, it was based on the rather incredible notion that all bodies respond roughly the same way to infection or injury, and the immune system is a well-organized defense mechanism that never attacks the body. This perspective is turning out to be oversimplified.
...
- “I wouldn’t be surprised if people are walking about with long Epstein-Barr virus, or long influenza. We all know someone who is low energy, who’s told to work harder. We have all heard about chronic-Lyme sufferers, and those with ME/CFS. But they get written off,” Spencer told me. The difference now is that it is happening “on such a huge scale—unlike anything we’ve seen before. It is harder for the medical community to write off.”
Kitty
Senior Member (Voting Rights)
But what on earth is she saying?
Codswallop?
Hoopoe
Senior Member (Voting Rights)
She appears to believe that ME sufferers believe in a postviral disease, while in her eyes long covid is viral and not postviral.
Also, the reason there has been lumping in ME is not for the lack of trying to split, but due to an inability to do so in a meaningful way.
Also, the reason there has been lumping in ME is not for the lack of trying to split, but due to an inability to do so in a meaningful way.
John Mac
Senior Member (Voting Rights)
Thanks for the translation into english @strategistShe appears to believe that ME sufferers believe in a postviral disease, while in her eyes long covid is viral and not postviral.
Also, the reason there has been lumping in ME is not for the lack of trying to split, but due to an inability to do so in a meaningful way.
Wyva
Senior Member (Voting Rights)
Bloomberg article:
Long Covid Is a Debilitating Mystery. Here’s What We Know
https://www.bloomberg.com/opinion/a...-s-what-we-know-about-covid-s-lasting-effects
The parts about ME/CFS:
Long Covid Is a Debilitating Mystery. Here’s What We Know
https://www.bloomberg.com/opinion/a...-s-what-we-know-about-covid-s-lasting-effects
The parts about ME/CFS:
The good news is that Long Covid sufferers are getting attention — there are some 70 Long Covid clinics around the U.K., and, according to NBC News, more than 80 post-Covid clinics in the U.S. This is a feat if you consider how relatively new Covid is. It took more than 80 years to determine a diagnosis for what’s known as Chronic Fatigue Syndrome or ME/CFS. Today it affects an estimated 2.5 million Americans and shares symptoms with Long Covid.
The costs of ignoring illness are high. ME/CFS sufferers have greater health care needs, are more likely to be unemployed, often require care from family members and are more likely to attempt suicide. Research into ME/CFS remains paltry, but sufferers are hoping that the interest in Covid’s after-effects will help shed new light on their own plight. Maybe they will get answers too. The U.S. National Institutes of Health has just announced funding worth $1.15 billion for investigations into Long Covid, which it has named Post-Acute Sequelae of Sars-CoV-2 or PASC.
Andy
Senior Member (Voting rights)
UK: Parliamentary hearing on long Covid and the need for it to be recognised as an occupational disease.
This took place today and is available on YouTube
Lucibee was presumably watching it and has tweeted some selected quotes, including this
and the APPG for Long Covid account tweeted this
This took place today and is available on YouTube
Code:
https://youtu.be/XK5Jz4Yqr8ALucibee was presumably watching it and has tweeted some selected quotes, including this
.@trishgreenhalgh says, "Show me someone with Long Flu..." err...
and the APPG for Long Covid account tweeted this
Dr David Strain @the BMA: To say Covid is like flu is absolutely ridiculous. As Trish said, you don’t get long flu.
Leila
Senior Member (Voting Rights)
I'm a member of a long covid support group here in Hungary and now that the covid situation is getting much worse than ever here (record high number of infections, much younger people with much worse symptoms than before with the new strains, etc), so now in the current situation I see desperate people, family members of young people with rapidly deteriorating condition, ask people with long covid to donate blood plasma, so more of it would be available for treating covid.
Do you have cases with severely affected LC people comparable with very severe ME? (completely bedbound, extreme sensitivity to light, sound, touch etc.)?
Wyva
Senior Member (Voting Rights)
I remember someone with LC in my own group who was completely bedbound first but then improved a lot. I saw some people who said walking is way too much for them. I don't know how common this is, it may not be. But when I came down with post-viral fatigue after glandular fever, I spent a lot of time on a gf forum and I remember reading everything but never commenting, because I didn't have the cognitive energy. People more severely affected may be less communicative and seemingly less present, who knows. Time will tell. But in general, this seems to be rare in the group.Do you have cases with severely affected LC people comparable with very severe ME? (completely bedbound, extreme sensitivity to light, sound, touch etc.)?
I haven't really seen people with sensory sensitivites but I think Scheibenbogen's recent study of people with LC mentioned that they found some people with that.
Edit: From that study:
These patients reported more fatigue in the Chalder Fatigue Score (p=0.006), more stress intolerance (p=0.042) and more frequent and longer post exertional malaise (PEM) (p=0.003), and hypersensitivity to noise (p=0.029), light (p=0.0143) and temperature (p=0.024) compared to patients not meeting ME/CFS criteria.
https://www.medrxiv.org/content/10.1101/2021.02.06.21249256v1
- Status
- Not open for further replies.

