I expected nothing better from Greenhalgh, it's still disappointing that they did not bother to learn a damn thing, still anchored on the invalid definition of ME as fatigue, THE fatigue. Nevermind that they say the same things for the same reasons and would explain the exact same way that LC is not just fatigue if one suggested so. Nevermind that it isn't really relevant what people "feel" is the cause of fatigue, even less so that it's a common thing to say for pwME that it an extreme level of fatigue unlike any normal fatigue, let alone that it's far far more than just that or even that PEM is obviously not the same as fatigue itself, even the extreme kind. Nevermind that dysautonomia causes fatigue and that it's very common in both. Nevermind it all. It's frankly getting silly, the level of willful ignorance, but that's just par for the course with us, we are not deserving of people actually being bothered by such things as facts like they normally do.
This paragraph is insulting. It was probably meant to be. Very silly to piss on our faces when all it does is splash back at them. It's entirely out of ignorance but it's still frustrating, as it's all coming at a time when it could have tipped the entire issue towards future progress given the NICE committee and whatever Cochrane is doing in the meantime waiting for others to absolve them of any responsibility in making a decision that will displease people irrelevant to the issue. Instead everything is stalemating. What a dumpster fire.
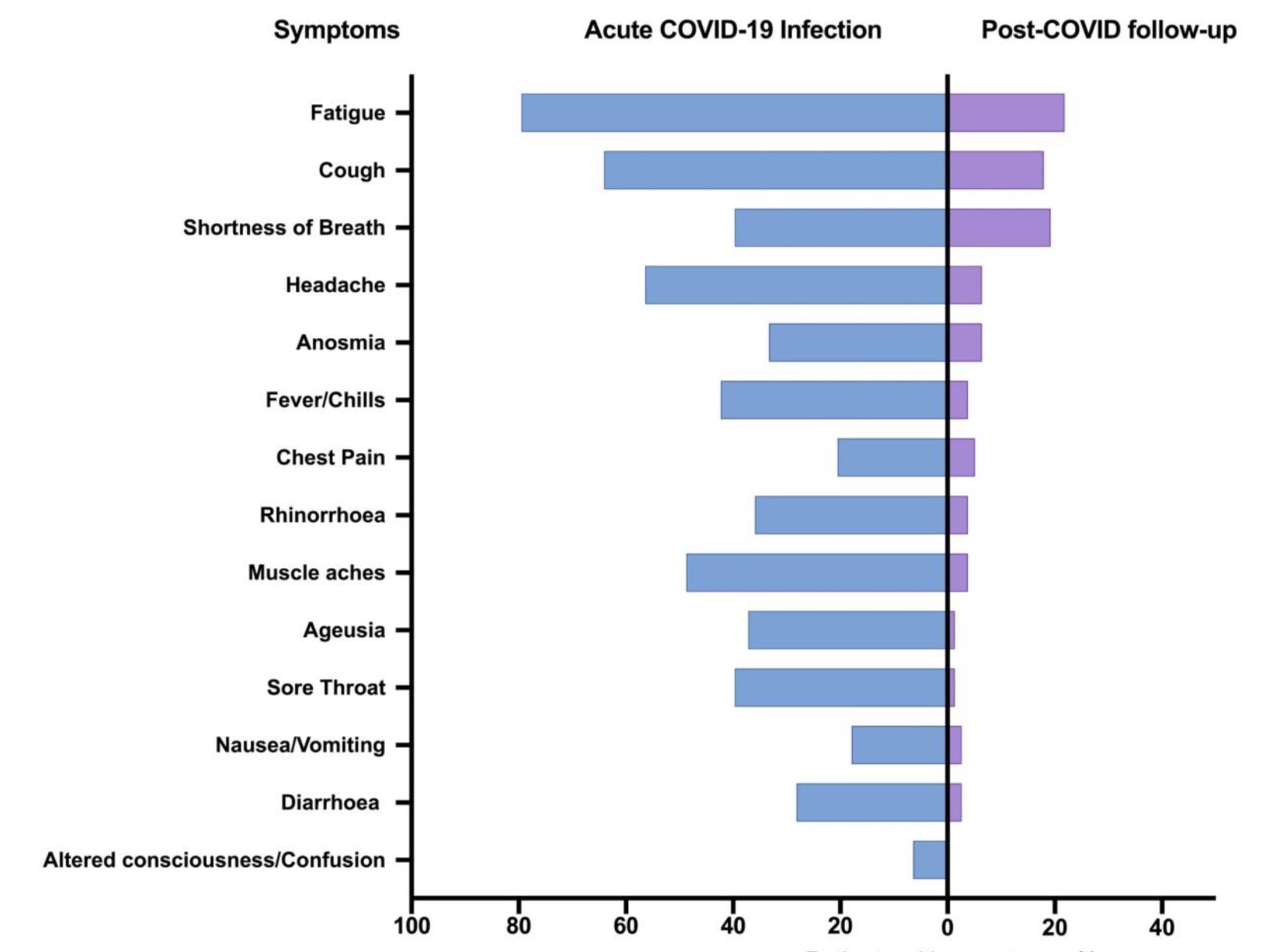
I browsed a bit. Of course if you'd remove the labels and context this may as well be an ME study. The statements and facts are the same. There is no mention of pacing, only one reference to exertion increasing symptoms, but as they did not bother to read anything about ME, of course they have no clue about PEM and since they shut the door on us they shut the door on this as well. Dumb dumb dumb and self-defeating.
I knew Greenhalgh would stab us in the face. Really silly that she and her team do not realize that in so off-handedly stabbing us without even looking back, they are also stabbing the LC in the back. Crabs in a bucket mentality meets escalation of commitment aligning to repeat the exact same mistakes for the exact same reasons. Frankly things are moving backwards right now, for everyone.
And nitpicky but one does not "express empathy". One either feels or has empathy and one expresses sympathy. Whatever.