Pretty impressive that you guys got this done in such a short period of time. You really put the Action into ME Action! Thanks also to Tom Kindlon for highlighting the responses in the appendices.
Here’s my view/summary of the survey.
Pressure to undergo certain treatments
The most striking figure for me was that 43.6% of 1340 respondents said they had been pressured to undergo a certain treatment. For children with ME and their carers this was figure was even higher, at 65% of 115 responses. One patient explained: “The pressure I felt to comply with treatment (GET) was subtle - I wasn't harassed into it but as I trusted the staff treating me I wanted to do my best to follow the programme even though I was clearly struggling.” Another patient said:
“I was put thorugh CBT which i did not want to do as it didn't work for me. I would go to appointments and be told if I didn't do the homework or didn't put in effort they would stop helping me and discharge me.”
Patients didn’t like CBT
Another notable figure: the majority (63%) of respondents (n= 551) did not find CBT helpful. And the people who did find it helpful seem to give reasons that suggest they received a different kind of CBT than the fear-avoidance version that is popular in the literature. For example, one person said
“Cbt helped me come to terms with having M.E. I'm not sure it helped with much else.”
We often describe CBT as psychological treatment. So people unaware of what CBT is, might think it involves talking therapy to help patients with their psychological problems. This isn’t always the case. CBT is mainly focused on cognitive restructuring, identifying and correcting unhelpful thoughts. From reading some of the comments I got the impression that some patients wanted someone to talk to about the problems ME/CFS had caused and that CBT didn’t fill that need. One patient even said:
“I was told I was 'too emotional' for CBT and that my ME was caused by depression because I cried in a session when talking about missing out on fun with my children. More emotional support is needed for people coping with ME because it can be isolating, lonely and depressing.”
Made me feel like a failure
From reading the comments I also got the impression that CBT can cause further psychological distress. One patient explained:
“CBT made no difference to the fatigue/PEM but left me feeling a bit of a failure as the psychologists view was that ‘this cure works’ so the fact that it hadn’t was down to me.” Another patient explained that
“the CBT message of pushing through which was playing like a destructive script in my head which reinforced a cycle of push and failure, push and failure. My self esteem was in tatters and it added a layer of stress on top.” The same was true for graded exercise therapy: patients too ill to follow the treatment were sometimes lead to believe they had done something wrong. One patient wrote:
“I was made to feel that failure to improve following this approach was down to a flaw in my personality- i.e. being too anxious and analytical- I realise now it was simply because I was too ill for GET.” Some patients were discouraged from seeking help or support or online:
“I was actively advised not to go online and seek support from charities and other groups, depending a sense of isolation and dependence on the service.”
Maintaining activity levels associated with harm
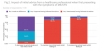
The survey did not have an assessment of GET but it did have interesting data on the initial advice patients got from a healthcare professional when they first presented with ME/CFS symptoms. Patients who were given the advice to increase or maintain activity levels when feeling ill report to have deteriorated much more than patients advised to rest or decrease their activity levels. The graph below is quite striking.
I personally suspect that surveys such as these are subject to selection bias: those who improved go on with their lives while those who had a bad experience are more willing to join a patient support group. So the people filling in these surveys are probably not representative of ME/CFS patients as a whole (the same is true for the patients in the randomized trials by the way). The differences in deterioration seen in this graph, however, are so striking that they probably cannot be fully explained by selection bias, at least that’s my impression. After all, it’s difficult to explain why patients told to rest or decrease their activity level when feeling unwell, report way less deterioration. There’s a ratio of approximately 1:10. So even if the respondents to the survey mostly represent those with a bad experience at the ME/CFS clinics, why do they say they deteriorated much worse with one advice and not the other? Perhaps one could argue there are some preconceptions that increasing activity when ill is bad for ME/CFS patients so patients might be more prone to attribute deterioration to such advice. Yet, the more modest advice to main activity levels whilst feeling ill is reported to be just as bad: almost 10x as many people report deterioration after this advice compared to the advice to rest or decrease activity levels.
False hope
From reading the comments, it seems that patients were given false hope about these treatments and that this was a reason they were willing to try and push try, even though this eventually made them worse. One patient said:
“6 years to get diagnosed, then when I did the clinic made me even worse, pushed me far beyond my body’s capabilities with the promise that I would recover from my deconditioning in their words.” Another patient commented:
“I was made to believe I had to keep pushing through. I did this for further 7/8years and believe I'm so much more worse for it. Its soul destroying.”
Not reporting harms
Another disturbing aspect that emerges from the comments is how badly the clinics sometimes responded to patients worsening during treatment. One patient explained:
“I was offered CBT and GET based on pacing but increasing. When I couldn't make it work the psychiatrist there wrote a letter to my GP criticising me for 'giving up easily'…" Another patient apparently had the same experience and wrote:
“The clinic sent a rude letter to my GP when he and I decided to stop intervention from the clinic because of my worsening condition. That affected how I was treated by other healthcare professionals and was very unprofessional.” Another patient commented:
“I was blamed for not improving because of GET, I said it was an improper treatment for me and they said ‘we get good results at this clinic’.” Someone else wrote:
“I did everything the 'experts' told me to do, deteriorated badly, and was discharged from the clinic because I wasn't improving.”
Another patient explained how she improved a little from medication she bought privately and that the clinic
“attributed this to their 'evidence-based treatment' which I hadn't even begun yet! Once I began their treatment I got significantly worse.” Another patient who described the treatment as harmful said:
“The clinic didn’t follow up why I dropped out or mention or monitor harm.” That’s in line with
a recent study by McPhee et al. who used freedom of information requests to show that ME/CFS clinics did not adequately monitor treatment harms.
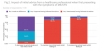
Pacing preferred over rest
The survey also asked patients what they thought, in hindsight, would be an appropriate advice. It seems that most patients prefer pacing (finding a sustainable daily activity level) rather than the advice to rest.
 Unsatisfied with the services
Unsatisfied with the services
Approximately half (52%) of the respondents were unsatisfied with ME/CFS services. Interestingly, one comment wrote:
“The staff were caring and obviously mean well. If the new NICE guidelines were less harmful/more helpful I am sure they would deliver them well. It is poor guidelines which cause the problems!” Most respondents thought that services should be led by a consultant like a neurologist or an immunologist, which isn’t always the case now. One patient wrote:
“I was diagnosed by a psychologist who never examined me. I have been unable to have further testing or treatments. I self-discharged as I was expending precious energy for no gain.” Another frequent comment is that the services were inaccessible to severe ME/CFS patients. One respondent wrote about their local ME/CFS service:
“It is not accessible by people severely affected at all. Not even by phone.”
No help at all
Just over a quarter of respondents (28.6%) had not been to an ME clinic. Many of the comments are about patients feeling abandoned by the medical community. One patient wrote:
“I am in my 12th year with m.e, and I feel like I have been left to rot by the medical profession.” Another patient wrote:
“I have been ill for 28 years, I live in Scotland but have NEVER been referred to any M.E/CFS services. I was just left to get on with it on my own.” Another comment says:
“I have not attended a clinic or specialist ME service because there isnt one. In almost 20 years I have had no specialised help or support from NHS. I cannot imagine there is another illness that is so life limiting that gets such little care.” There was also this sad but charming comment from a husband and wife who both have ME:
“My husband has ME too- we got it after bad infection in Jan 1995. Life has been very hard. We feel alone but there must be other couples with it surely? We would have made a brilliant longitudinal study but have had to 'hide' from a critical society, medical establishment, employer and governments for so long. Please remember those who have had this for yearsthe walking dead. Ageing and it's greater opportunity to rest is not giving the relief we had hoped for - we are simply older with ME now!”