Dx Revision Watch
Senior Member (Voting Rights)
I haven't been able to find an archived English language edition of WHO's unmodified ICD-8, yet.
But the German DIMDI site has archived facsimile German language versions of ICD-8 Tabular list and Index that can be downloaded as PDFs from very large Zip files:
https://www.dimdi.de/dynamic/de/klassifikationen/downloads/?dir=icd-vorrevisionen
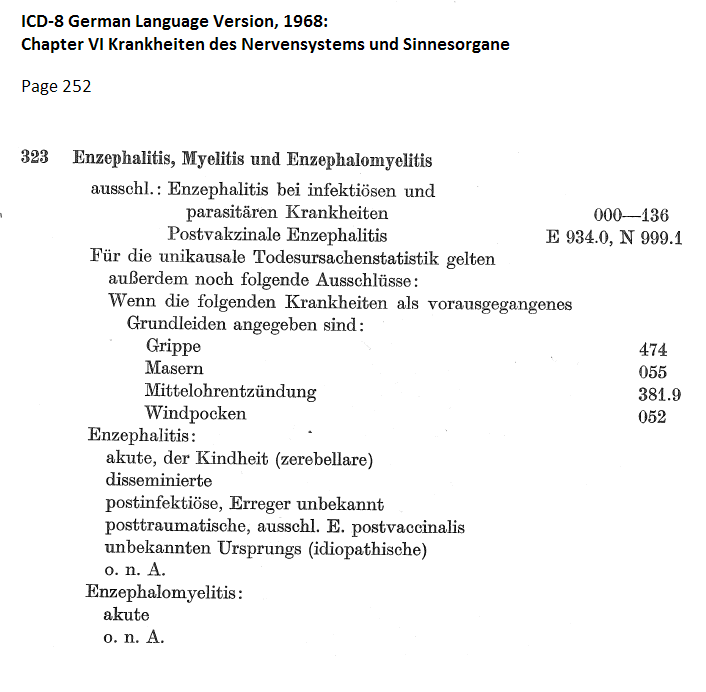
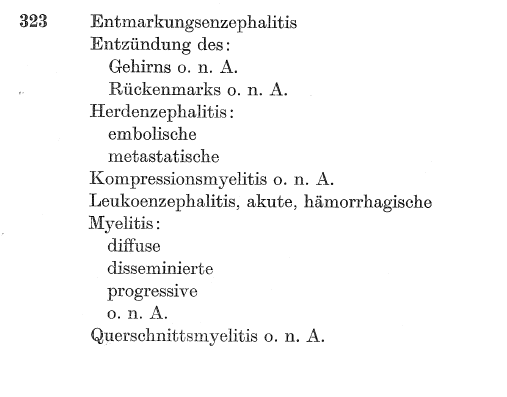
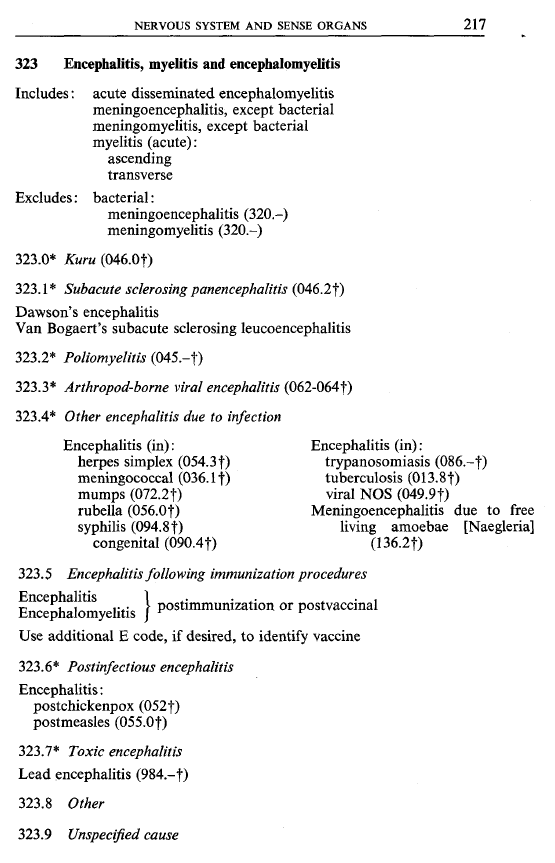
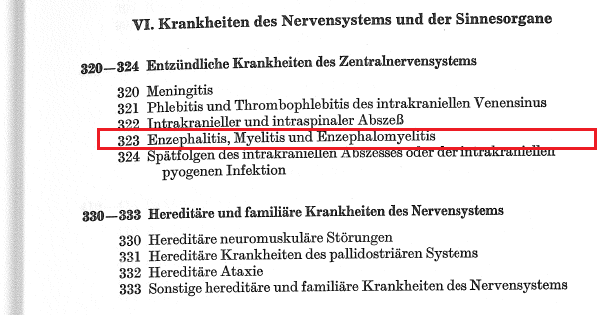
Here is a screenshot from Chapter VI
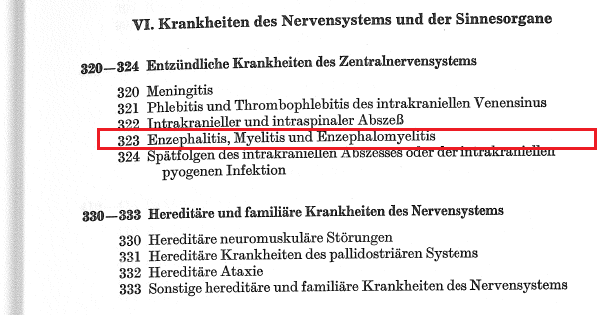
Again, no inclusion under the code
323 Enzephalitis, Myelitis und Enzephalomyelitis
for Myalgische Enzephalomyelitis or [German translation of Benign] Myalgische Enzephalomyelitis.
Nor can I see any "Myalgische Enzephalomyelitis" in the Index that is indexed to code 323.
OK, this a German language version of ICD-8 but I remain to be convinced that the term "Benign myalgic encephalomyelitis" or "Myalgic encephalomyelitis" was included in ICD-8 at code 323.
Although 323 Encephalitis, myelitis and encephalomyelitis was.
But the German DIMDI site has archived facsimile German language versions of ICD-8 Tabular list and Index that can be downloaded as PDFs from very large Zip files:
https://www.dimdi.de/dynamic/de/klassifikationen/downloads/?dir=icd-vorrevisionen
Here is a screenshot from Chapter VI
Again, no inclusion under the code
323 Enzephalitis, Myelitis und Enzephalomyelitis
for Myalgische Enzephalomyelitis or [German translation of Benign] Myalgische Enzephalomyelitis.
Nor can I see any "Myalgische Enzephalomyelitis" in the Index that is indexed to code 323.
OK, this a German language version of ICD-8 but I remain to be convinced that the term "Benign myalgic encephalomyelitis" or "Myalgic encephalomyelitis" was included in ICD-8 at code 323.
Although 323 Encephalitis, myelitis and encephalomyelitis was.
Last edited: