If you are not happy with the proposal to add a Symptom chapter code for
post-exertional malaise (PEM)/post-exertion symptom exacerbation (PESE) to the US's ICD-10-CM, there is still time to submit comments and concerns.
Send your comments via email to CDC by Friday, May 5.
https://meglobalchronicle.wordpress...myalgic-encephalomyelitis-me-using-icd-codes/
ME Global Chronicle
BURYING MYALGIC ENCEPHALOMYELITIS (ME) USING ICD CODES
Published: 23 April 2023
Colleen Steckel
Independent US advocate
Due to the potential harm which could come from the proposal to add a symptom code for post-exertional malaise (PEM)/post-exertion symptom exacerbation (PESE), I have decided to submit the following comment to
nchsicd10CM@cdc.gov.
Deadline for comments is May 5, 2023.
To:
nchsicd10CM@cdc.gov
I do not support adding a symptom code for PEM/PESE.
The proposal to add R68.A could lead to tracking data for myalgic encephalomyelitis being further lost. As it stands now, the G93.32 code has become muddied by electronic health record systems expanding how it is used.
By creating a symptom code for PEM/PESE doctors could opt to use their preferred code of chronic fatigue, unspecified (R53.82) along with this new PEM/PESE code instead of G93.32. This coding approach would further bury the ability to track myalgic encephalomyelitis.
Alternatively doctors may diagnose with diseases they are more familiar with that are often seen in our charts like fibromyalgia, postural orthostatic tachycardia syndrome, orthostatic intolerance, depression etc., in conjunction with PEM/PESE instead of diagnosing ME.
In order to make sure those who have Long COVID with PEM/PESE are most accurately tracked, I recommend giving those with Long COVID who have PEM/PESE a unique diagnosis code. I suggest U09.91 be used to enable tracking these patients as a distinct group. A specific code for this subset of Long COVID patients is required if they are going to get the most effective research and treatment protocol as quickly as possible.
Colleen Steckel
Independent patient/advocate myalgic encephalomyelitis
Background
Why diagnosis codes matter
1. Ability to track how many people have ME
2. Ability to track how many people die from ME
3. Ability to get appropriate care covered by insurance
4. Ability to get disability benefits
Proposal to add new symptom code R68.A
In March, a proposal was submitted by Long COVID advocates to NCHS/CDC to add a code for post-exertional malaise/post exertion symptom exacerbation (PEM/PESE) to the US healthcare system, ICD-10-CM. The new code, if approved, would be R68.A.
We have all seen the challenges that come with trying to get a diagnosis of myalgic encephalomyelitis. Most doctors prefer to use the less controversial codes like chronic fatigue, unspecified (R53.82) or codes that focus on one aspect of ME. For instance, those with pain are often labeled with fibromyalgia. Doctors may also focus on the dysautonomia symptoms and code accordingly.
Because of this tendency to avoid the G93.32 code, concerns have been raised that the addition of a symptom code for PEM/PESE may compound this problem. Up until now, patients who have symptoms of orthostatic intolerance, pain, and cognitive issues combined with PEM/PESE could point their doctors to the G93.32 code because that is the only code that encompasses PEM/PESE.
The potential to cause harm may be that doctors will rely on the more common codes like chronic fatigue, unspecified or fibromyalgia and then just combine those with the PEM/PESE code.
This may lead to those with ME being categorized outside of the G93.32 code. The result being that ME would become even more invisible.
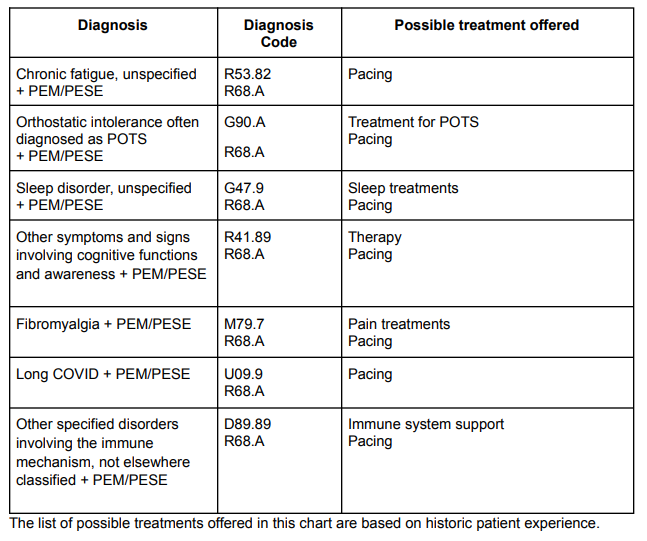
The following chart shows how a medical provider could code patients without using ME/CFS.
The list of possible treatments offered in this chart are based on historic patient experience.
In the US, ICD codes are also used for decisions made by insurance companies about what care is covered. To learn more about concerns about this proposal to add PEM/PESE to the US ICD codes, please read
HERE.
This proposal is discussed at Science for ME beginning
HERE.
Submit your comments about this proposal by May 5, 2023 to
nchsicd10CM@cdc.gov
Problems with G93.32
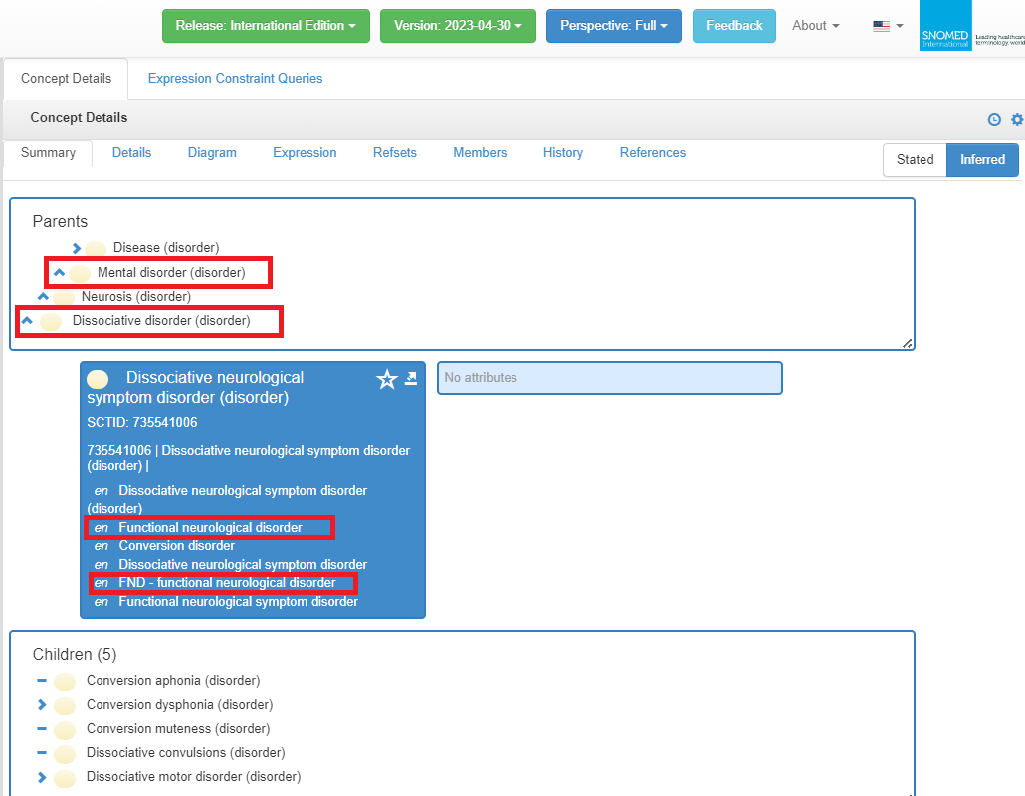
The following explains how G93.32 is now being used for more than just ME, ME/CFS and CFS.
Outside of the US, tracking information has not been available for myalgic encephalomyelitis separate from chronic fatigue syndrome because the World Health Organization combines both under the G93.3 code.
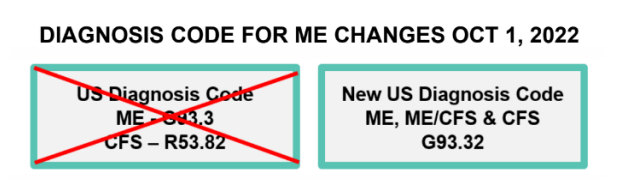
In the US, up until October 2022, ME was coded G93.3 and CFS was coded in the Symptoms, signs chapter under R53.82. After October 1, 2022, ME, CFS & ME/CFS were all combined under G93.32. Read about that change
HERE.
Continued in Part Two.