The Long Covid group "Patient-Led Research Collaborative", with support from #MEAction, Open Medicine Foundation, Solve ME/CFS Initiative, Massachusetts ME/CFS & FM Association, and Pandora Org has submitted a proposal to the March 7-8 ICD-10-CM Coordination and Maintenance Committee (C&M):
https://patientresearchcovid19.com/storage/2022/10/Post-exertional-malaise-ICD-10-Proposal.pdf
Patient-Led Research Collaborative
To: National Center for Health Statistics
From: Patient-Led Research Collaborative, with support from #MEAction, Open Medicine Foundation, Solve ME/CFS Initiative, Massachusetts ME/CFS & FM Association, and Pandora Org
Subject: ICD code for post-exertional malaise/post-exertional symptom exacerbation Date: June 10, 2022
The majority of Long COVID patients experience an exacerbation of some or all of their symptoms and a further reduction in functioning following physical or cognitive exertion or emotional, positional, sensory, or other stressors. 1-3 This symptom, referred to as post-exertional malaise (PEM) and post-exertional symptom exacerbation (PESE), is characterized by: 4-7
● Exacerbation of some or all of a patient’s symptoms or occurrence of new symptoms. Symptoms exacerbated can include physical fatigue, cognitive fatigue, exercise intolerance, problems thinking (e.g. slowed information processing speed, memory, concentration), unrefreshing sleep, muscle pain, joint pain, headaches, weakness/instability, light-headedness, flu-like symptoms, sore throat, nausea, orthostatic intolerance or other autonomic dysfunctions, sensory sensitivities, and other symptoms.
● Pathological loss of stamina and/or functional capacity that is not due to physical deconditioning 5,8
● An onset that can be immediate or delayed after the exertional stimulus by hours to days
● A prolonged, unpredictable time to return to baseline that is not easily relieved by rest or sleep and may last days, weeks, months, or longer
● Severity and duration of symptoms that is often out-of-proportion to the type, intensity, frequency, and/or duration of the exertion
Even basic activities of daily living like toileting, bathing, dressing, communicating, and reading can trigger PEM/PESE. In some instances, the specific precipitant cannot be identified. The threshold for a precipitant to trigger PEM/PESE can vary between individuals as well as within the same individual, at different times during their illness.
This symptom has important implications for Long COVID diagnosis, treatment, disability assessment, morbidity tracking, and research using electronic health records. For instance:
● In its guidance on fatigue and recommendations for exercise, the American Academy of Physical Medicine and Rehabilitation discusses the importance of identifying PEM and cautions against exercise programs that provoke PEM. 9 The World Physiotherapy, a coalition of physical therapy associations from around the world, issued similar recommendations in its COVID briefing paper to prevent harm to patients. 10
● PEM/PESE needs to be evaluated and considered in recommendations for accommodations and in disability claims because of its significant impact over days or longer on a patient’s ability to work or attend school. 11,12
● Numerous Long COVID studies, including those in NIH’s RECOVER Initiative and by the CDC, are now using electronic health records to identify important sequelae of an acute SARS CoV-2 infection. 13,14 PEM/PESE is virtually invisible in these studies.
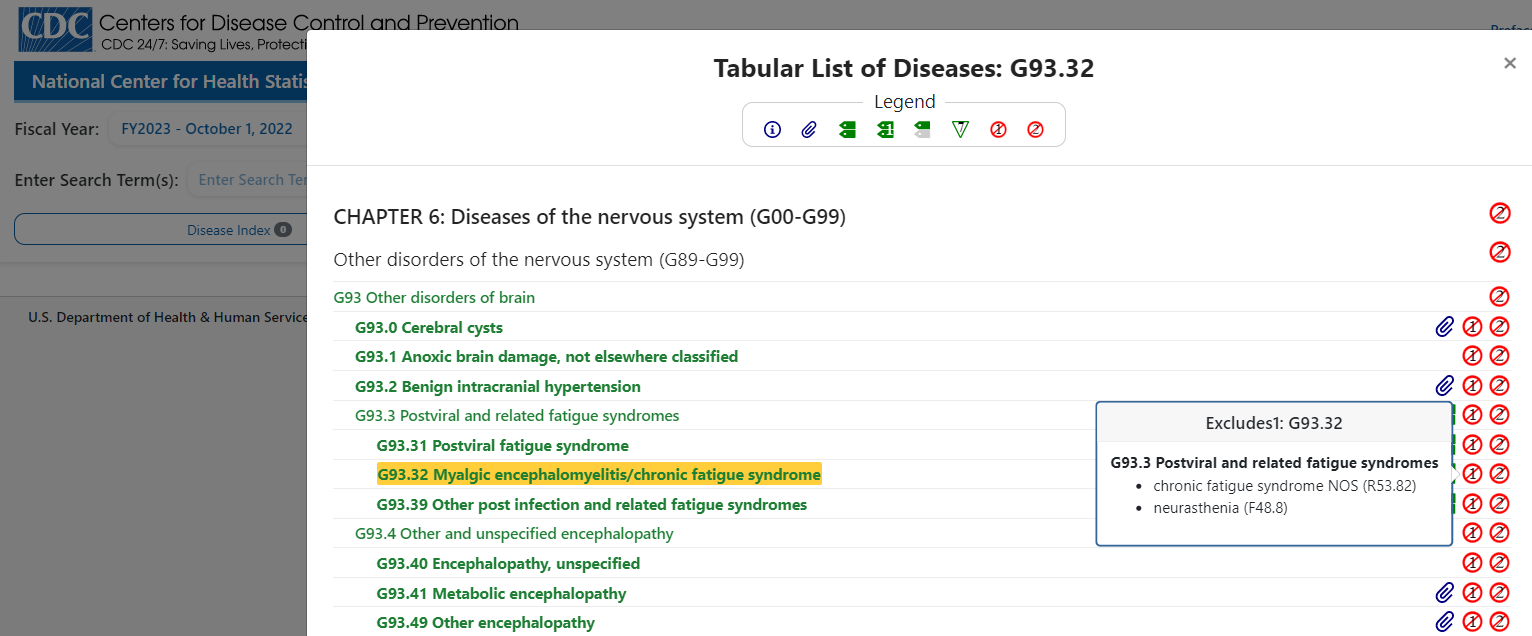
Currently, the ICD-10-CM does not have a code for the symptom of PEM/PESE as described for Long COVID and myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS).
As a result, this important symptom is not being identified or tracked in electronic health records or in morbidity tracking systems. A code for PEM/PESE is needed to rectify this issue. This would also facilitate education of physicians, improve communication between a patient and clinician and between the PCP and other healthcare providers, and improve the accuracy of Long COVID research using electronic health records.
It’s important to note that while PEM is included in a diagnosis of ME/CFS, 4 not all patients with Long COVID and PEM/PESE have been given an ME/CFS diagnosis, either because the patient has not yet met the 6 month diagnostic requirement of ME/CFS in adults 4 or because the patient does not meet the other ME/CFS criteria. Thus, a code for the symptom of PEM/PESE separate from a diagnosis of ME/CFS is required.
Further, while much of the existing literature on the symptom references PEM, we ask that PESE be included as an inclusion term, or be considered for the lead term, as PESE has started to be used by the patient and research community alike. 10,15 This is because it more accurately reflects patients’ experience of the symptom - an exacerbation of a host of symptoms as opposed to solely the experience of malaise. We ask that this new code
be implemented no later than Spring of 2023. Expedited implementation is required because of the magnitude of the affected patient population and to ensure the accurate tracking of this important sequelae and the accuracy of current and ongoing research using electronic health records like in the RECOVER Initiative.
Please contact Lisa McCorkell (lisa@patientledresearch.com) with any questions or to discuss this or alternative approaches to achieving the objective of tracking the important symptom.
The following changes are recommended to capture the symptom of PEM/PESE:
TABULAR MODIFICATIONS
R68 Other general symptoms and signs
Add R68.4 Post-exertional malaise
Post-exertional symptom exacerbation
PEM
PESE
Post-exertional neuroimmune exhaustion
Note:
Due to “malaise” being in the name of PEM, NCHS may be considering placing PEM under R53. However, PEM has been incorrectly conflated with fatigue. PEM is an exacerbation of some or all symptoms and a further reduction in functioning and should be categorized in another section to avoid reinforcing this misunderstanding.
References etc.
[Full document attached]