Andy
Senior Member (Voting rights)
Day two now available, https://videocast.nih.gov/launch.asp?27424
The entire first day is available to stream on demand, https://videocast.nih.gov/launch.asp?27422
No individual talks or timestamps for individual talks available yet.
They can also be downloaded for offline viewingDay two now available, https://videocast.nih.gov/launch.asp?27424
https://www.medscape.com/viewarticle/911666 - may need free sign up to view.New Findings Elucidate Potentially Treatable aspects of ME/CFS
Bethesda, MD — New evidence of cardiopulmonary and nervous system abnormalities in people with myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) yields clues to the etiology of their exercise intolerance and points to potential treatments.
The findings were presented during the 2-day Accelerating Research on ME/CFS Meeting sponsored by the National Institutes of Health (NIH) and held on its main campus. The meeting brought together researchers from a range of scientific and clinical disciplines along with patients and patient advocates.
During cycling, many ME/CFS patients will have relatively normal VO2 max levels but abnormally low filling pressure, particularly the right atrial pressure. That phenomenon, which Systrom and colleagues have called "preload failure," is seen in nearly all patients evaluated with iCEPT who meet ME/CFS criteria.
In a study Systrom and colleagues published in 2016 on 49 patients with this phenomenon, giving two saline boluses corrected the problem in most cases. The authors concluded that inadequate ventricular filling related to low venous pressure is a clinically relevant cause of exercise intolerance. "In retrospect, most of those patients had evidence of ME/CFS," he observed.
@Jonathan Edwards remember that you were skeptical about IV saline?
(I'm not sure if you were concerned about potential harm from having an infusion as opposed to just drinking salt water, or skeptical about the idea that salt water would be genuinely helpful)
Surface interactions of EVs with the plasma membrane are of outstanding importance since such interactions mediate binding of EVs to cells resulting in signal transduction or uptake of EVs by cells. It is now established that EV-target cell interactions involve tetraspanins, integrins, ECM proteins, immunoglobulin superfamily members, proteoglycans, and lectins [21, 22]. Details of EV docking and entry to cells are not in the focus of this review, as these interactions have recently been reviewed elsewhere [21, 22]. To illustrate the outstanding functional significance of the interaction of EV surface molecules with those of the plasma membrane, here, we only refer to the plethora of EV-immune cell interactions including cell-free antigen presentation by EVs [23], Fas ligand or TRAIL-mediated cell death induction by EVs
[24–26], or the transfer of immune checkpoint molecules (PD1, PDL-1) by EVs
I personally think there was really nothing there in the Montoya cytokine results... all moderate patients were no different than controls. I’m not sure I buy this bimodal explanation either.
What do people think? I’m sure it was talked about here when the paper came out. Cytokines are a tricky business to measure accurately and reproducibly and technology might need to improve before we see anything.
@FMMM1 on a minor point of accuracy, the UK had a Labour Government from 1997 to 2010, and the PACE trial ran between 2005 and 2010, so I assume the funding was agreed while Labour was in power, not the Conservatives.
The NICE guidelines, in their current format i.e. CBT and GET as treatments, come from 2007, so before PACE. PACE will have reinforced the thinking behind them but it didn't result in any change of policy by itself.I hadn't known that. However, the decision to implement policy (GET/CBT), based on the PACE trial, was I assume made after the publication of the trial results - in the Lancet in February 2011 [https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(11)60096-2/fulltext].
The decision to implement a policy/not to implement a policy (GET/CBT) was therefore made by the incoming Conservative Government.
Action for ME acted as the secretariat to the all party parliamentary group on ME and supported the implementation of GET/CBT as a treatment for ME - stating that there was evidence (PACE) that it helped some people.
https://www.sierranevada.edu/2019-valedictorian-eva-jazbec/During the past four years, I spent 7 semesters tutoring math and science at SNC. I interned at the UC Davis TERC Chemistry Lab for 9 months, where I contributed to the long-term monitoring dataset on Lake Tahoe water quality. For the past 12 months, I’ve been conducting clinical research on patients with Chronic Fatigue Syndrome at Simmaron Research.
Simmaron is an Incline Village scientific non-profit which focuses on identifying promising new avenues for CFS research. I was fortunate enough to receive the National Institute of Health (NIH) travel award to attend a workshop for young/early career ME/CFS investigators. I also presented my data as a poster co-author at the NIH conference: “Accelerating Research on Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS)”.
The NICE guidelines, in their current format i.e. CBT and GET as treatments, come from 2007, so before PACE. PACE will have reinforced the thinking behind them but it didn't result in any change of policy by itself.
The guidelines are determined by NICE, theoretically an independent body, so to claim that any UK government, Conservative or Labour, implemented treatment policy will be an unhelpful statement to make, in my opinion.
Cort's summary of the conference - Day 1:
Accelerating ME/CFS: The NIH Conference Day 1
Is this serum switching (healthy cells in sick serum vs sick cells in healthy serum) independent of Davis' research? Would be pretty strong boost to have honed in on the same observation.
Can we/should we/will we now start lobbying, e.g. through ME Action - Millions Missing, for the development of a diagnostic test based on this and the assessment of potential treatments (SS31)? The people who influence health research spending aren't likely to read what's on this site; we should try to speak to those people i.e. EU MEPs/UK MPs
https://www.meaction.net/2019/02/26/announcing-millionsmissing-2019-join-us/Each demonstration should decide what targets (it can be general or specific) will be most impactful for drawing attention at your location. We aren’t dictating specific targets this year by country as we did in previous years. In the UK and Scotland, the #MillionsMissing campaign will focus on increasing funding for biomedical research into the diagnosis and treatment of ME.
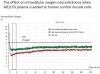
Three independent teams, using three different methods, with the same result.The first group who identified this were, as Bhupesh Prusty acknowledges earlier in his talk, Fluge/Mella (December 2016). Fluge/Mella used a Seahorse analyser which measures cellular energy metabolism i.e. by measuring "oxygen consumption rate (OCR) and extracellular acidification rate (ECAR)". Subsequently Ron Davis found the same effect using the nano-needle (which measures impedance).
What Bhupesh has done is measured this in an entirely different way i.e. by measuring mitochondrial fragmentation - in that sense it is entirely different from the Seahorse analyser/nano-needle.
What he also appears to have done is established what changes in the cells mitochondria (i.e. mitochondrial fragementation) and suggested the mechanism(?) i.e. microRNA. So presumably everyone is no going to try to get money for looking for microRNAs (i.e. which fragment mitochondria) in exosomes - is Maureen Hanson already doing this?