Also from the thread:
Thread: MUS, PPS services and IAPT integration into NHS primary care - what's happening across the UK?
https://forums.phoenixrising.me/thr...ening-across-the-uk.48710/page-21#post-806218
Just to complicate matters:
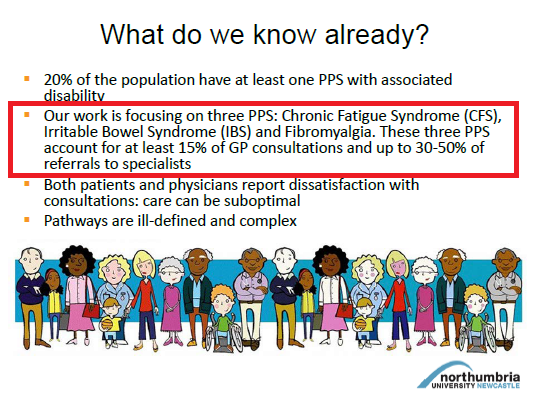
In England, we are increasingly seeing the term "medically unexplained symptoms" deprecated in favour of the term "Persistent physical symptoms (PPS)".
In Scotland, "Persistent physical symptoms" is being used, on this site at least, where the term, "long-term conditions (LTCs)" is used in England.
http://www.nes.scot.nhs.uk/educatio...ogical-interventions-and-physical-health.aspx
NHS Education for Scotland
Quality Education for a Healthier Scotland
Psychological Interventions and Physical Health
NES Psychology directorate has been developing a programme of work aimed at addressing the training needs of the NHS Scotland workforce in relation to psychological interventions in physical health care...
(...)
https://www.ucl.ac.uk/pals/research...ople_with_Persistent_Physical_Health_Problems
The Matrix (2015) A Guide to Delivering Evidence-Based Psychological Therapies in Scotland; Persistent Physical Symptoms
The Psychological Therapies 'Matrix' is a guide to planning and delivering evidence-based Psychological Therapies within NHS Boards in Scotland. The Matrix is published by NES, in partnership with the Scottish Government. It provides a summary of the information on the current evidence base for various therapeutic approaches, guidance on well functioning psychological therapies services and advice on important governance issues. The sub-section relating to the psychological management of persistent physical symptoms was updated in 2015.
Persistent Physical Symptoms refers to health problems that last a year or longer, impact on a person’s life, and may require ongoing care and support. The definition does not relate to any one condition, care group or age category. Common examples include diabetes, heart disease, chronic pain, arthritis, inflammatory bowel disease, asthma and chronic obstructive pulmonary disease (COPD).
The evidence tables for persistent physical symptoms can be found and downloaded in the link below:
http://www.nes.scot.nhs.uk/media/3500010/matrix_-_persisent_physical_symptomstablesfinal_1.pdf
The document in the PDF:
(My highlighting)
Psychosocial Interventions for People with Persistent Physical Symptoms
Introduction
Persistent Physical Symptoms, refers to health problems that last a year or longer, impact on a
person’s life, and may require ongoing care and support.
The definition does not relate to any one
condition, care group or age category. Common examples include diabetes, heart disease, chronic pain,
arthritis, inflammatory bowel disease, asthma and chronic obstructive pulmonary disease (COPD).
Around 2 million people in Scotland have at least one such condition, and one in four adults over
16 years reported some form of long term illness, health problem or disability, and one in five have
chronic pain. These conditions become more common with age. By the age of 65, nearly two-thirds
of people will have developed Persistent Physical Symptoms, however, more people under the age of
65 years in Scotland have multiple conditions.
(...)
Asthma
Cancer
Cardiovascular disease (CVD)
Chronic fatigue syndrome (CFS)
Chronic kidney disease
Chronic obstructive pulmonary disease (COPD)
Chronic pain
Diabetes Type 1 and Type 2
Irritable bowel syndrome (IBS)
Multiple sclerosis (MS)
Osteoarthritis
Rheumatoid arthritis
Obesity/Weight loss interventions
But in England, PPS is being used for:
"Medically unexplained symptoms"
under which is also included, in some cases:
Fibromyalgia
Irritable Bowel Syndrome
Chronic Fatigue Syndrome/ ME
Functional Neurological Symptoms (including Non-Epileptic Attacks)
The NHS Education for Scotland site has a separate page for MUS:
http://www.nes.scot.nhs.uk/educatio...chology/mus-long-term-conditions-toolkit.aspx
MUS - Long Term Conditions Toolkit
The term “medically unexplained symptoms” is used to describe a set of persistent physical symptoms (e.g. chest pain, dizziness, back pain) for which, after extensive investigation, there is no obvious underlying cause or diagnosis.
For those with persistent physical symptoms, the journey from symptom development to clear understanding and evidence-based treatment can be an arduous one. In an attempt to exclude more concerning underlying conditions, GPs often undertake a range of medical assessments and interventions.
While necessary, these can cause patients to develop:
- unwanted psychological and physical side effects, adding to distress and disability
- beliefs about the nature and seriousness of their condition,
- Additional pain, fatigue and other symptoms due to pharmacological interventions.
In the absence of a clear cause or diagnosis despite persisting symptoms, patients can become increasingly distressed, while fear of what may be generating symptoms often leads to avoidance of daily activities. Further investigations may also place the patient at risk of harm, for instance, due to infection from exploratory operations, and exceeding safe doses of radiation etc.