Sly Saint
Senior Member (Voting Rights)
Defining the minimally clinically important difference of the SF-36 physical function subscale for paediatric CFS/ME: triangulation using three different methods
https://link.springer.com/article/10.1186/s12955-018-1028-2
Abstract
Background
Defining the minimally clinically important difference (MCID) is important for the design and analysis of clinical trials and ensures that findings are clinically meaningful. Studies in adult populations have investigated the MCID of The Short Form 36 physical function sub-scale (SF-36-PFS). However, to our knowledge no studies have defined the MCID of the SF-36-PFS in a paediatric population. We aimed to triangulate findings from distribution, anchor and qualitative methods to identify the MCID of the SF-36-PFS for children and adolescents with CFS/ME.
Methods
Quantitative methods: We analysed routinely-collected data from a specialist paediatric CFS/ME service in South-West England using: 1) the anchor method, based on Clinical Global Impression (CGI) outcomes at 6 months’ follow-up; 2) the distribution method, based on the standard deviation of baseline SF-36-PFS scores.
Qualitative methods: Young people (aged 12–17 years) and parents were asked to complete the SF-36-PFS, marking each question twice: once for where they would currently rate themselves/their child and a second time to show what they felt would be the smallest amount of change for them/their child to feel treatment had made a difference. Semi-structured interviews were designed to explore what factors were deemed important to patients and to what extent an improvement was considered satisfactory. We thematically analysed qualitative interviews from 21 children and their parents.
Results
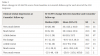
Quantitative results: Six-month follow-up data were available for 198 children with a mean age of 14 years. Most were female (74%, 146/198) and 95% gave their ethnicity as “White British”.
Half the standard deviation of the baseline SF-36-PFS scores was 11.0. “A little better” on the CGI equated to a mean difference on the SF-36-PFS from baseline to 6-month follow-up of 9.0.
Qualitative results: Twenty-one children with CFS/ME participated: 16 females (76.2%) with a mean age of 14.4 years. Twenty mothers and two fathers were also interviewed.
The median minimal improvement in the SF-36-PFS was 10. Participants indicated that small changes in physical function can lead to important improvements in valued social and family function. Patients and parents were positive about improvement even in the presence of persisting symptoms.
Triangulation: The MCID based on the mean score from the three methods was 10.
Conclusions
Converging evidence indicates future studies in paediatric CFS/ME should use an MCID of 10 on the SF-36-PFS.
Keywords
Minimal clinically important difference (MCID) Paediatric Chronic fatigue syndrome Myalgic encephalomyelitis CFS/ME
Abbreviations
CFS/ME
Chronic Fatigue Syndrome / Myalgic Encephalomyelitis
CGI
Clinical Global Impression Scale
MCID
Minimal Clinically Important Difference
SF-36-PFS
The SF-36 physical function sub-scale
https://doi.org/10.1186/s12955-018-1028-2) contains supplementary material, which is available to authorized users.
https://link.springer.com/article/10.1186/s12955-018-1028-2