Circulating Levels of SMPDL3B Define Metabolic Endophenotypes and Subclinical Kidney Alterations in Myalgic Encephalomyelitis
Myalgic Encephalomyelitis (ME) is a complex, multisystem disorder with poorly understood pathophysiological mechanisms. SMPDL3B, a membrane-associated protein expressed in renal podocytes, is essential for lipid raft integrity and glomerular barrier function. We hypothesize that reduced membrane-bound SMPDL3B may contribute to podocyte dysfunction and impaired renal physiology in ME.
To investigate this, we quantified soluble SMPDL3B in plasma and urine as a surrogate marker of membrane-bound SMPDL3B status and assessed renal clearance and plasma metabolomic profiles
In a cross-sectional study of 56 ME patients and 16 matched healthy controls, ME patients exhibited significantly lower urine-to-plasma ratios of soluble SMPDL3B and reduced renal clearance, suggesting podocyte-related abnormalities. Plasma metabolomics revealed dysregulation of metabolites associated with renal impairment, including succinic acid, benzoic acid, phenyllactic acid, 1,5-anhydroglucitol, histidine, and citrate.
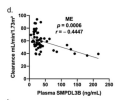
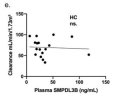
In ME patients, plasma SMPDL3B levels inversely correlated with 1,5-anhydroglucitol concentrations and renal clearance. Multivariable modeling identified the urine-to-plasma SMPDL3B ratio as an independent predictor of clearance. Female ME patients showed more pronounced SMPDL3B alterations, reduced clearance, and greater symptom severity. Non-linear associations between soluble SMPDL3B and lipid species further suggest systemic metabolic remodeling.
These findings support soluble SMPDL3B as a potential non-invasive biomarker of renal-podocyte involvement in ME, highlighting sex-specific differences that may inform future therapeutic strategies.
Web | PDF | International Journal of Molecular Sciences | Open Access
Rostami-Afshari, Bita; Elremaly, Wesam; McGregor, Neil R; Huang, Katherine Jin Kai; Armstrong, Christopher W; Franco, Anita; Godbout, Christian; Elbakry, Mohamed; Abdelli, Rim; Moreau, Alain
Myalgic Encephalomyelitis (ME) is a complex, multisystem disorder with poorly understood pathophysiological mechanisms. SMPDL3B, a membrane-associated protein expressed in renal podocytes, is essential for lipid raft integrity and glomerular barrier function. We hypothesize that reduced membrane-bound SMPDL3B may contribute to podocyte dysfunction and impaired renal physiology in ME.
To investigate this, we quantified soluble SMPDL3B in plasma and urine as a surrogate marker of membrane-bound SMPDL3B status and assessed renal clearance and plasma metabolomic profiles
In a cross-sectional study of 56 ME patients and 16 matched healthy controls, ME patients exhibited significantly lower urine-to-plasma ratios of soluble SMPDL3B and reduced renal clearance, suggesting podocyte-related abnormalities. Plasma metabolomics revealed dysregulation of metabolites associated with renal impairment, including succinic acid, benzoic acid, phenyllactic acid, 1,5-anhydroglucitol, histidine, and citrate.
In ME patients, plasma SMPDL3B levels inversely correlated with 1,5-anhydroglucitol concentrations and renal clearance. Multivariable modeling identified the urine-to-plasma SMPDL3B ratio as an independent predictor of clearance. Female ME patients showed more pronounced SMPDL3B alterations, reduced clearance, and greater symptom severity. Non-linear associations between soluble SMPDL3B and lipid species further suggest systemic metabolic remodeling.
These findings support soluble SMPDL3B as a potential non-invasive biomarker of renal-podocyte involvement in ME, highlighting sex-specific differences that may inform future therapeutic strategies.
Web | PDF | International Journal of Molecular Sciences | Open Access