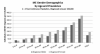
I don't think anyone here is surprised by this. The graph of diminishing income is quite similar to my own, with many years where it was zero. And many continuous months in the years before of on/off work.
I would confidently assert that everyone dealing with this, from our biopsychosocial overlords to government authorities and anyone working in psychosomatic ideology is well aware of this. The main, hell the only, purpose of those rehabilitation programs is to get us back to work. That they choose to focus on secondary analyses of various mental health labels changes nothing to the fact that the aim of those programs would frame it as a rousing success if most of us got back to work but our mental health deteriorated sharply as a result, however unlikely that may be.
And knowing of the failure of those programs, essentially spending money to lose more money, is precisely why there is so much hostility towards us. They are making the exact same calculation as the famous quote from Fight Club, a true devil's bargain:
- Narrator: A new car built by my company leaves somewhere traveling at 60 mph. The rear differential locks up. The car crashes and burns with everyone trapped inside. Now, should we initiate a recall? Take the number of vehicles in the field, A, multiply by the probable rate of failure, B, multiply by the average out-of-court settlement, C. A times B times C equals X. If X is less than the cost of a recall, we don't do one.
- Woman on Plane: Are there a lot of these kinds of accidents?
- Narrator: You wouldn't believe.
- Woman on Plane: Which car company do you work for?
- Narrator: A major one.
Their rehabilitation programs are both a gross and a net loss. But they calculate that the cost to them is lower than the full cost of acknowledging the illness, paying full disability for everyone affected, and having to conduct research solving this intractable problem. IMO every country, health care system and health authority makes this calculation knowing that if they ever choose to end the policy of "I reject reality and substitute my own", they alone would bear the cost of doing so, because it's very unlikely that anyone would follow them at it. They know that efforts so far have come up bust and that it would take a major international research effort to solve it, and that those almost never happen in medical research. It's a complete scattershot effort with zero coordination or economies of scale.
So they don't do the recall. They let us burn and crash at enormous costs to everyone, mainly to us but also massively expensive to society, because they don't have confidence in the institutions of medicine and the tools of science to do what they do best: solve complex problems. This attitude is so common, the learned helplessness they have all accepted in full: what if we try and if it's for nothing because there's nothing and we look like fools for having tried, for being suckers who fell for a bunch of worried-whiners?
Of course there's a self-fulfilling prophecy part of this because of delayed diagnoses, which although on paper at 6 months, is actually closer to the 5-6 years mark, not accounting for those who never get diagnoses. This is largely why almost no one here recovers, because it's a process that no one knows how to affect, so when it happens it's a natural organic thing, but by delaying diagnoses they make sure that they mostly see patients past the point of no return. Even though a full count would still have to account for lots of people being out of work, likely labeled 'burnout' or mild depression or whatever, for months or years.
And of course LC is changing this by going the other way around and targeting those least disabled and within the main period of recovery, so that they can boast about recoveries they had nothing to do with. Which all distorts everything back, but of course making a true comparison between patients who go through rehabilitation and those who don't would show no difference between the group, with likely slightly worse odds in the active rehabilitation cohorts. As long as they don't actually count, they can maintain their denial of reality.
I just can't imagine, given how easy it is to get this information, that those involved in this are not aware of this. They are certainly the kinds of fools who fool themselves first, but the data don't lie. This is why almost none of the trials, and none of the clinics, despite existing solely for the purpose of getting people back to work, report this. Why PACE reported their null results in another paper published in a lesser journal.
More of this kind of research, please. This is what exposes the lies. The programs only exist to get us back to work. They don't do that. All the money spent on those are wasted twice over with us being unable to work anyway, and all of this in addition to base expenses that go into raising someone to a functioning adult: all the education, health care and various expenses that get repaid during a lifetime of paying taxes. It's the absolute worst lose-lose-lose-lose proposition and this is how their lies get exposed: with dollar/euro/currency signs.