You are using an out of date browser. It may not display this or other websites correctly.
You should upgrade or use an alternative browser.
You should upgrade or use an alternative browser.
USA Centers for Disease Control (CDC) news (including ME/CFS Stakeholder Engagement and Communication Calls)
- Thread starter Sasha
- Start date
Dolphin
Senior Member (Voting Rights)
Recently released information on CDC ME/CFS Stakeholder callCDC ME/CFS Program Update has just been posted in advance of today's meeting
https://www.cdc.gov/me-cfs/pdfs/23-sec-cdc-program-update-5-3-24.pdf
Slides [for "Clinical Manifestations and pathophysiology of #LongCOVID" by Avi Nath]
https://www.cdc.gov/me-cfs/pdfs/23-sec-call-covid-cdc-slides-508.pdf
Transcript
https://www.cdc.gov/me-cfs/media/pdfs/2024/06/23-SEC_-May-6-2024_-Transcript_-FINAL.pdf
Dolphin
Senior Member (Voting Rights)
Source: CDC
MECFS-SEC
Date: October 16, 2024
Author: Dana Brimmer
URL: mailto:MECFSSEC@cdc.gov
CDC ME/CFS Call December 4, 2024 3:00pm ET
------------------------------------------
CDC ME/CFS Stakeholder Engagement and Communication (SEC) Conference
Call.
Participants can join the call using zoom by clicking on the Link OR
copying and pasting it into your web browser.
Participants can join the zoom webinar by clicking this link:
https://cdc.zoomgov.com/j/1612754572?pwd=EPxMfvWuzHjEbrPF1kZ2SHFFwksqjo.1
When the zoom page opens,
* click on the 'launch meeting' button,
* enter your email address and name, then
* click on the 'join webinar' button.
Participants can also join by phone using the following number (when
prompted, please enter the meeting id and passcode):
* TELEPHONE: 1-669-254-5252
* MEETING ID: 161 275 4572
* PASSCODE: 12116411
Meeting Agenda
--------------
Welcome and Meeting Overview
Updates from CDC
Elizabeth Unger, PhD, MD
Branch Chief, Chronic Viral Diseases Branch, Centers for Disease Control
and Prevention
'A Primer About POTS'
Satish Raj, M.D.
Professor of Cardiac Science, Libin Cardiovascular Institute and the
University of Calgary's Cumming School of Medicine, University of
Calgary, Canada
Question and Answer (Q&A)
To ask a question during the meeting within the Zoom webinar platform,
please:
* Click on the 'Raise Hand' button.
* Ask your question when prompted.
To ask a question during the meeting by phone, please:
* Enter *9 to add yourself to the queue.
* Ask your question when prompted.
Closed captioning will be provided the week before the call.
More information about CDC SEC Calls can be found at the CDC ME/CFS
website.
https://www.cdc.gov/me-cfs/events/?CDC_AAref_Val=https://www.cdc.gov/me-cfs/programs/meetings.html
MECFS-SEC
Date: October 16, 2024
Author: Dana Brimmer
URL: mailto:MECFSSEC@cdc.gov
CDC ME/CFS Call December 4, 2024 3:00pm ET
------------------------------------------
CDC ME/CFS Stakeholder Engagement and Communication (SEC) Conference
Call.
Participants can join the call using zoom by clicking on the Link OR
copying and pasting it into your web browser.
Participants can join the zoom webinar by clicking this link:
https://cdc.zoomgov.com/j/1612754572?pwd=EPxMfvWuzHjEbrPF1kZ2SHFFwksqjo.1
When the zoom page opens,
* click on the 'launch meeting' button,
* enter your email address and name, then
* click on the 'join webinar' button.
Participants can also join by phone using the following number (when
prompted, please enter the meeting id and passcode):
* TELEPHONE: 1-669-254-5252
* MEETING ID: 161 275 4572
* PASSCODE: 12116411
Meeting Agenda
--------------
Welcome and Meeting Overview
Updates from CDC
Elizabeth Unger, PhD, MD
Branch Chief, Chronic Viral Diseases Branch, Centers for Disease Control
and Prevention
'A Primer About POTS'
Satish Raj, M.D.
Professor of Cardiac Science, Libin Cardiovascular Institute and the
University of Calgary's Cumming School of Medicine, University of
Calgary, Canada
Question and Answer (Q&A)
To ask a question during the meeting within the Zoom webinar platform,
please:
* Click on the 'Raise Hand' button.
* Ask your question when prompted.
To ask a question during the meeting by phone, please:
* Enter *9 to add yourself to the queue.
* Ask your question when prompted.
Closed captioning will be provided the week before the call.
More information about CDC SEC Calls can be found at the CDC ME/CFS
website.
https://www.cdc.gov/me-cfs/events/?CDC_AAref_Val=https://www.cdc.gov/me-cfs/programs/meetings.html
Last edited:
Dolphin
Senior Member (Voting Rights)
This is on in less than 24 hours wherever you are in the world.Source: CDC
MECFS-SEC
Date: October 16, 2024
Author: Dana Brimmer
URL: mailto:MECFSSEC@cdc.gov
CDC ME/CFS Call December 4, 2024 3:00pm ET
------------------------------------------
CDC ME/CFS Stakeholder Engagement and Communication (SEC) Conference
Call.
Participants can join the call using zoom by clicking on the Link OR
copying and pasting it into your web browser.
Participants can join the zoom webinar by clicking this link:
https://cdc.zoomgov.com/j/1612754572?pwd=EPxMfvWuzHjEbrPF1kZ2SHFFwksqjo.1
When the zoom page opens,
* click on the 'launch meeting' button,
* enter your email address and name, then
* click on the 'join webinar' button.
Participants can also join by phone using the following number (when
prompted, please enter the meeting id and passcode):
* TELEPHONE: 1-669-254-5252
* MEETING ID: 161 275 4572
* PASSCODE: 12116411
Meeting Agenda
--------------
Welcome and Meeting Overview
Updates from CDC
Elizabeth Unger, PhD, MD
Branch Chief, Chronic Viral Diseases Branch, Centers for Disease Control
and Prevention
'A Primer About POTS'
Satish Raj, M.D.
Professor of Cardiac Science, Libin Cardiovascular Institute and the
University of Calgary's Cumming School of Medicine, University of
Calgary, Canada
Question and Answer (Q&A)
To ask a question during the meeting within the Zoom webinar platform,
please:
* Click on the 'Raise Hand' button.
* Ask your question when prompted.
To ask a question during the meeting by phone, please:
* Enter *9 to add yourself to the queue.
* Ask your question when prompted.
Closed captioning will be provided the week before the call.
More information about CDC SEC Calls can be found at the CDC ME/CFS
website.
https://www.cdc.gov/me-cfs/events/?CDC_AAref_Val=https://www.cdc.gov/me-cfs/programs/meetings.html
Dolphin
Senior Member (Voting Rights)
A 5-page CDC ME/CFS program update https://www.cdc.gov/me-cfs/media/pdfs/2024/12/SEC_Call_December-4_CDC_Program_Update_Clean_Final.pdf has just been posted to the CDC website https://www.cdc.gov/me-cfs/events/index.html in advance of the meeting in less than 2 hours.
Last edited:
Dolphin
Senior Member (Voting Rights)
I used this and wasn't asked for a passcode:I'm having trouble with the passcode not being right, have others got in ok with that passcode?
https://cdc.zoomgov.com/j/1612754572?pwd=EPxMfvWuzHjEbrPF1kZ2SHFFwksqjo.1
(Thanks. I was joining from my browser, as I hadn't updated my zoom version, and with that the screen asking for the passcode appeared. When I updated my zoom version the screen asking for a passcode did not appear. It's odd as the Cdc did provide a passcode, it just didn't work.)
Last edited:
I was doing something else while listening, so I don't have much in the way of notes.
On the CDC update, I missed that, so I'm just going off the pdf provided before the meeting. At 5 pages, it's not so long to read but here's a summary and some comments on some interesting things there:
As part of the CDC's educational programme, they had an event for nursing students at the Emory School of Nursing which they organised in conjunction with MEAction Georgia. While the event sounds good, but the scale of effort seems off by an order of magnitude. I don't know if the session was recorded?
I can't recall what we have thought about the study, but a biobank and databank available to researchers sounds like a good initiative.
More from the MCAM study:
Cognitive assessment in ME/CFS: a cognitive substudy of the multi-site clinical assessment of ME/CFS (MCAM), 2024, Lange, Unger +
National Association of School Nurses
CDC has a contract with the NASN, and here it does seem as though there is a good level of effort in educating medical professionals. They say they have reached 40,000 school nurses with educational materials during the 3 year NASN partnership, and 11,000 school nurses have undertaken CPD on ME/CFS in the past year.
ICUE
STOP ME/CFS project
CDC is working with the Emerging Infections Program in California and Kaiser Permanente Northern California. Work on quantifying the incidence of ME/CFS has been published. The study is ongoing.
Long COVID and Fatiguing Illness Recovery Program
COVID-RELIEF Project
My sense is of some reasonable initiatives, but it's all very piecemeal, small and preliminary. Also, a lot of things that are Long Covid are now being counted as ME/CFS effort. Which is fair enough I guess, but the combined effort surely needs to be much bigger than this. Where is the national effort on accurate coding so that the size of the problem can really be seen? Where is the CDC's effort to prevent more people getting LC-ME/CFS?
If anyone from the CDC reads this, it would be great if they could include hyperlinks to the research and webinars that they mention in their pre-meeting transcript. It would save people a lot of time hunting around for research, given that they often don't give very good identifying information.
On the CDC update, I missed that, so I'm just going off the pdf provided before the meeting. At 5 pages, it's not so long to read but here's a summary and some comments on some interesting things there:
A new person in the CDC ME/CFS team. That's an interesting background, with rickettsias, Ebola and MERS all implicated in the triggering of ME/CFS.I would like to welcome Joanna Regan, as our new medical officer and team lead working on ME/CFS. Joanna is trained as a pediatrician and also has a master’s in public health. She came to work at CDC in 2009 in the Rickettsial Zoonoses Branch as a medical officer. Her past work at CDC has included investigations on an outbreak of Rocky Mountain spotted fever, and on Ebola and Middle East Respiratory Syndrome. She has worked with health departments and traveled tomore than 20 countries for CDC. We are excited to have Joanna as part of CDC’s ME/CFS program.
As part of the CDC's educational programme, they had an event for nursing students at the Emory School of Nursing which they organised in conjunction with MEAction Georgia. While the event sounds good, but the scale of effort seems off by an order of magnitude. I don't know if the session was recorded?
MCAM = Multi-site Clinical Assessment of ME/CFS studyWe are thrilled to announce that an extensive collection of more than 70 datasets and biospecimens from MCAM are now accessible through the websites mapMECFS and searchMECFS, respectively. Applications for data use and biospecimens are approved through data use agreements.
I can't recall what we have thought about the study, but a biobank and databank available to researchers sounds like a good initiative.
More from the MCAM study:
we published “Chronic Overlapping Pain Conditions in People with Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS): A Sample from the Multi-Site Clinical Assessment of ME/CFS (MCAM) Study,” and “Cognitive Assessment in Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS): A Cognitive Sub-study of the Multi-Site Clinical Assessment of ME/CFS (MCAM)
75% of people with ME/CFS had at least one of the following chronic overlapping pain conditions: chronic low back pain, chronic migraines or headaches, fibromyalgia, interstitial cystitis or irritable bowel syndrome, or temporomandibular disorder.
Those findings about cognition are very interesting - I'll link the studies if I can find them. Edit - Here it is:In the cognitive study, we found processing speed was significantly lower for people with ME/CFS when compared to healthy controls. We also found that the challenges associated with a clinic visit that includes cognitive testing worsened processing speed to the same extent as exercise testing.
Cognitive assessment in ME/CFS: a cognitive substudy of the multi-site clinical assessment of ME/CFS (MCAM), 2024, Lange, Unger +
National Association of School Nurses
CDC has a contract with the NASN, and here it does seem as though there is a good level of effort in educating medical professionals. They say they have reached 40,000 school nurses with educational materials during the 3 year NASN partnership, and 11,000 school nurses have undertaken CPD on ME/CFS in the past year.
Additionally, we have tracked absences for over 15,000 students, identifying that approximately 3% were due to ME/CFS-related symptoms. In October, we began the next phase and aim to expand our data collection efforts across eight more states.
ICUE
This seems to have involved some webinars, and some collaboration with patient organisations.In October, we wrapped up our partnership project, “Infection-Associated Chronic Conditions— Understanding and Engagement,” also known as ICUE.
...CDC Foundation’s lead partner organizations, Solve M.E., the COVID-19 Longhauler Advocacy Project, and the Patient-Led Research Collaborative hosted the final webinar
STOP ME/CFS project
CDC is working with the Emerging Infections Program in California and Kaiser Permanente Northern California. Work on quantifying the incidence of ME/CFS has been published. The study is ongoing.
Overall, the researchers estimated that 1.67%, or 45,892, of 2.7 million adult KPNC members of the Kaiser plan in Northern California had ME/CFS-like syndrome during the study period, which was July to October 2022. Of those, 14% developed the illness after COVID-19.
Long COVID and Fatiguing Illness Recovery Program
I copied that out in full. It sounds positive. Of course, it depends a lot on what the webinars are saying, but at least they are mentioning post-exertional malaise. I wonder why the CDC hasn't focussed on improving medical training i.e. getting the doctors and nurses informed before they face patients. I wonder how big that primary care clinician support program (ECHO) is.We are also continuing our work to educate primary care providers about Long COVID, ME/CFS and other post-acute infection syndromes through the Long COVID and Fatiguing Illness Recovery Program. This project is a collaboration with one of the largest federally qualified health centers, the Family Health Centers of San Diego, along with the ECHO Institute at the University of New Mexico, and the Schools of Medicine at the University of Washington, and the University of Colorado. In this third year of the program, our collaborators have continued to host monthly webinars for continuing medical education credit. From the program’s inception, the webinars have included presentations and discussion by both medical and lived experience experts (meaning either a patient or patient caregiver). In the past 6 months, webinars have covered recent research findings and other topics such as the diagnosis of post-exertional malaise and Long COVID Patient Navigation. Beginning November 7, the program expanded the opportunity to enroll in monthly case-consultation and mentoring through the ECHO online platform to primary care clinicians nationwide. On November 14, the program’s 10th online short course for CME credit, called “Long COVID in Children and Adolescents,” was posted.
COVID-RELIEF Project
Finally, in early November, we published a paper resulting from the COVID-RELIEF Project, our collaboration with the University of Washington, in BMC Infectious Diseases.The paper describes quality of life impairments and subjective cognitive decline associated with Long COVID two or more years after the patients’ initial SARS-CoV-2 infection.
My sense is of some reasonable initiatives, but it's all very piecemeal, small and preliminary. Also, a lot of things that are Long Covid are now being counted as ME/CFS effort. Which is fair enough I guess, but the combined effort surely needs to be much bigger than this. Where is the national effort on accurate coding so that the size of the problem can really be seen? Where is the CDC's effort to prevent more people getting LC-ME/CFS?
If anyone from the CDC reads this, it would be great if they could include hyperlinks to the research and webinars that they mention in their pre-meeting transcript. It would save people a lot of time hunting around for research, given that they often don't give very good identifying information.
Last edited:
On Dr Satish Raj's presentation:
It was an interesting presentation. I think it's worth a listen by anyone interested in orthostatic intolerance in ME/CFS. He comes across as trying his best for his patients, and engaging in research to try to answer questions about treatments.
Dr Raj distinguished POT(the symptom) from POTS (the syndrome). He notes that POT occurs in most people when they have a viral infection. I think that's a really interesting observation. Why does that happen? Is it part of the engineered sickness response, to get people fighting an infection to stop, lie down and direct energy resources to getting well? How does it work?
He also notes that fatigue tends to be ubiquitous in people presenting with POTS, even if they don't meet ME/CFS criteria.
He said that POTS isn't really a fainting disorder, people just feel very unwell. He said that in a recent tilt table test study, more POTS patients completed the test than controls did. They felt really bad, but they didn't faint, perhaps because the tachycardia was compensating/responding to the physiological challenge.
There was an interesting section on whether patients with POTS are more anxious than normal. Dr Raj's wife is a psychiatrist and she she looked at this question. She found that the POTS patients were more anxious than the healthy controls, but they weren't more anxious than the population in general. She found that the healthy controls in the study were actually hyper-mentally well (or I guess at least reported being so). It could be worth finding that study, Raj et al 2009. It's a good point to remember - there is selection bias in the controls as well as the patients.
Dr Raj noted that a diagnosis of POTS is like a diagnosis of a fever - lots of causes, and the right treatment depends on the cause. Doctors should be trying to find the cause.
Okamoto 2012 study - looked at the overlap of POTS and ME/CFS - and found a substantial overlap.
Garland 2012 study - looked at the effect of salt. Dr Raj says that the study found that a high sodium diet did increase plasma volume, reduced plasma norepinephrine and decreased standing heart rate. There was a trend to reduced symptoms. He recommends it to his patients.
Bourne et al 2021 and a new one Bourne et al 2024 - looked at the effect of compression garments. Found they do work, especially garments that compress the abdomen, where most of the blood pooling occurs.
He also mentions exercise as useful, especially recumbent exercise. And also that there are medications.
He says that all of these are management tools that can help, even perhaps help a lot, but they are not cures.
Now I'd like to introduce our guest speaker. Dr. Satish Raj is a Heart Rhythm Cardiologist. He completed his internal medicine and cardiology training at Queen’s University, and then further trained in cardiac electrophysiology at the University of Calgary. He then spent 12 years working at the Vanderbilt Autonomic Dysfunction Center in Nashville, Tennessee. He is currently Professor of Cardiac Science at the Libin Cardiovascular Institute and the University of Calgary’s Cumming School of Medicine and founder of the Calgary Autonomic Investigation & Management Clinic. His primary research interests relate to understanding and better treating postural tachycardia syndrome (POTS), vasovagal syncope, and orthostatic hypotension. He is conducting studies into the role of autoantibodies and inflammation in POTS and understanding the “brain fog” of POTS. He is also looking at repurposing drugs in novel ways to treat vasovagal syncope and orthostatic hypotension. Welcome, Dr. Raj.
It was an interesting presentation. I think it's worth a listen by anyone interested in orthostatic intolerance in ME/CFS. He comes across as trying his best for his patients, and engaging in research to try to answer questions about treatments.
Dr Raj distinguished POT(the symptom) from POTS (the syndrome). He notes that POT occurs in most people when they have a viral infection. I think that's a really interesting observation. Why does that happen? Is it part of the engineered sickness response, to get people fighting an infection to stop, lie down and direct energy resources to getting well? How does it work?
He also notes that fatigue tends to be ubiquitous in people presenting with POTS, even if they don't meet ME/CFS criteria.
He said that POTS isn't really a fainting disorder, people just feel very unwell. He said that in a recent tilt table test study, more POTS patients completed the test than controls did. They felt really bad, but they didn't faint, perhaps because the tachycardia was compensating/responding to the physiological challenge.
There was an interesting section on whether patients with POTS are more anxious than normal. Dr Raj's wife is a psychiatrist and she she looked at this question. She found that the POTS patients were more anxious than the healthy controls, but they weren't more anxious than the population in general. She found that the healthy controls in the study were actually hyper-mentally well (or I guess at least reported being so). It could be worth finding that study, Raj et al 2009. It's a good point to remember - there is selection bias in the controls as well as the patients.
Dr Raj noted that a diagnosis of POTS is like a diagnosis of a fever - lots of causes, and the right treatment depends on the cause. Doctors should be trying to find the cause.
Okamoto 2012 study - looked at the overlap of POTS and ME/CFS - and found a substantial overlap.
Garland 2012 study - looked at the effect of salt. Dr Raj says that the study found that a high sodium diet did increase plasma volume, reduced plasma norepinephrine and decreased standing heart rate. There was a trend to reduced symptoms. He recommends it to his patients.
Bourne et al 2021 and a new one Bourne et al 2024 - looked at the effect of compression garments. Found they do work, especially garments that compress the abdomen, where most of the blood pooling occurs.
He also mentions exercise as useful, especially recumbent exercise. And also that there are medications.
He says that all of these are management tools that can help, even perhaps help a lot, but they are not cures.
Last edited:
Maybe because patients have had experience with and practice at managing POTS? They are better at reading the somatic signs, and judging how far they can push it before needing to sit/lie down?He said that POTS isn't really a fainting disorder, people just feel very unwell. He said that in a recent tilt table test study, more POTS patients completed the test than controls did. They felt really bad, but they didn't faint, perhaps because the tachycardia was compensating/responding to the physiological challenge.
Thanks Hutan, those were interesting comments. Eg the controls being uber-controls and not representative of the general population; the fact that controls would faint far more often than POTS patients (who felt terrible but were compensating); and the compression-wear being effective at the abdomen, not the lower limbs.
I'll post some of those papers you mentioned in a bit.
Edit: we had most, here are the thread links —
A Community-Based Trial of Commercially Available Compression Tights in Patients With Postural Orthostatic Tachycardia Syndrome (2024, Clinical Electrophysiology)
Compression Garment Reduces Orthostatic Tachycardia and Symptoms in Patients With Postural Orthostatic Tachycardia Syndrome (2021, Journal of the American College of Cardiology)
Salt supplementation in the management of orthostatic intolerance: Vasovagal syncope and postural orthostatic tachycardia syndrome (2022, Autonomic Neuroscience)
Dietary sodium and health: How much is too much for those with orthostatic disorders? (2022, Autonomic Neuroscience)
Effect of High Dietary Sodium Intake in Patients With Postural Tachycardia Syndrome (2021, Journal of the American College of Cardiology)
I'll post some of those papers you mentioned in a bit.
Edit: we had most, here are the thread links —
A Community-Based Trial of Commercially Available Compression Tights in Patients With Postural Orthostatic Tachycardia Syndrome (2024, Clinical Electrophysiology)
Compression Garment Reduces Orthostatic Tachycardia and Symptoms in Patients With Postural Orthostatic Tachycardia Syndrome (2021, Journal of the American College of Cardiology)
Salt supplementation in the management of orthostatic intolerance: Vasovagal syncope and postural orthostatic tachycardia syndrome (2022, Autonomic Neuroscience)
Dietary sodium and health: How much is too much for those with orthostatic disorders? (2022, Autonomic Neuroscience)
Effect of High Dietary Sodium Intake in Patients With Postural Tachycardia Syndrome (2021, Journal of the American College of Cardiology)
Last edited:
Ebb Tide
Senior Member (Voting Rights)
This is one study on anxiety in POTS by Dr Raj's wife-not sure if the same one mentioned in the post above by @Hutan
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2758320/?tool=pubmed
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2758320/?tool=pubmed
Dolphin
Senior Member (Voting Rights)

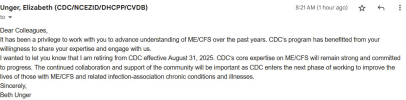
It's ME(Jaime) (@exceedhergrasp1.bsky.social)
Beth Unger is retiring from work with #MECFS at #CDC.
ETA: I’ll try embedding a post from X:
It's ME(Jaime) (@exceedhergrasp1.bsky.social)
Beth Unger is retiring from work with #MECFS at #CDC.bsky.app
Last edited:
ME/CFS Science Blog
Senior Member (Voting Rights)
Dolphin
Senior Member (Voting Rights)

It's ME(Jaime) (@exceedhergrasp1.bsky.social)
Beth Unger is retiring from work with #MECFS at #CDC.bsky.app
ETA: I’ll try embedding a post from X:
From Solve ME:
Today, we join the #MECFS community in expressing our deep gratitude to Dr. Beth Unger, who has led the CDC’s Chronic Fatigue Syndrome Program with dedication and compassion.
Her leadership helped:
From all of us at Solve M.E. and the ME/CFS community: Thank you, Dr. Unger.
We also want to take a moment to acknowledge the recent tragedy at the CDC and extend our heartfelt support to our colleagues there as they process and heal.
Read our full open letter here: https://ow.ly/Im0a50WGS3m
wigglethemouse
Senior Member (Voting Rights)
X is blocked on s4me for me so this was the full quote on X giving context.We also want to take a moment to acknowledge the recent tragedy at the CDC and extend our heartfelt support to our colleagues there as they process and heal.
"We also want to take a moment to acknowledge the recent shooting at the CDC and send our heartfelt support to our colleagues there as they process and heal from this tragedy. Our thoughts are with all those affected"
Dolphin
Senior Member (Voting Rights)
Dolphin
Senior Member (Voting Rights)
Source: U.S. Federal Register
Vol. 91, #28, pp 6219-6221
Date: February 11, 2026
URL:
https://www.federalregister.gov/doc...mitted-for-public-comment-and-recommendations
https://www.govinfo.gov/content/pkg/FR-2026-02-11/pdf/2026-02654.pdf
[A Notice by the Centers for Disease Control and Prevention]
Proposed Data Collection Submitted for Public Comment and
Recommendations
-------------------------------------------------------------------------
This document has a comment period that ends in 61 days (04/13/2026)
AGENCY: Centers for Disease Control and Prevention (CDC), Department of
Health and Human Services (HHS).
ACTION: Notice with comment period.
SUMMARY: The Centers for Disease Control and Prevention (CDC), as part
of its continuing effort to reduce public burden and maximize the
utility of government information, invites the general public and other
federal agencies the opportunity to comment on a proposed and/or
continuing information collection, as required by the Paperwork
Reduction Act of 1995. This notice invites comment on a continuing
information collection project titled School-Based Active Surveillance
(SBAS) of Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS)
Among Schoolchildren. This project will expand on the work from previous
phases for active surveillance of chronic conditions, including ME/CFS
and other infection associated chronic conditions and illnesses (IACCs),
using an electronic data collection platform.
DATES: CDC must receive written comments on or before April 13, 2026.
ADDRESSES: You may submit comments, identified by Docket No.
CDC-2026-0166 by either of the following methods:
* Federal eRulemaking Portal: http://www.regulations.gov. Follow the
instructions for submitting comments.
* Mail: Jeffrey M. Zirger, Information Collection Review Office, Centers
for Disease Control and Prevention, 1600 Clifton Road NE, MS H21-8,
Atlanta, Georgia 30329.
Instructions: All submissions received must include the agency name and
Docket Number. CDC will post, without change, all relevant comments to
http://www.regulations.gov.
Please note: Submit all comments through the Federal eRulemaking portal
(http://www.regulations.gov) or by U.S. mail to the address listed
above.
FOR FURTHER INFORMATION CONTACT: To request more information on the
proposed project or to obtain a copy of the information collection plan
and instruments, contact Jeffrey M. Zirger, Information Collection
Review Office, Centers for Disease Control and Prevention, 1600 Clifton
Road NE, MS H21-8, Atlanta, Georgia 30329; Telephone: 404-639-7570;
Email: omb@cdc.gov.
(...)
Background and Brief Description
Myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS), a complex,
chronic, debilitating multi-system disease, affects up to 3.3 million
persons in the United States. However, about 90% of people with ME/CFS
have not received an official diagnosis from a healthcare professional.
ME/CFS affects between 0.10% and 0.75% of children and adolescents,
which often goes undiagnosed by healthcare professionals.
Data on chronic conditions among schoolchildren, such as asthma, has
been collected over the years, but there has been little to no emphasis
on ME/CFS in the United States. Chronic conditions among school-aged
children likely account for a high proportion of chronic school
absenteeism and school withdrawal. Conducting active surveillance among
students using school nurses could expedite the diagnosis and management
of children who present with symptoms commonly seen in ME/CFS. This
involves educating school nurses about ME/CFS and its related syndromes,
how to best approach parents and guardians when suggesting the
diagnosis, and how to support the educational success of students with
chronic diseases.
National active surveillance in schools for ME/CFS coupled with
education of school nurses about ME/CFS could help improve measuring the
burden of ME/CFS in children and provide insights for future plans to
improve healthcare in children suffering from ME/CFS and other chronic
health conditions. In the next phase of this project, we will expand the
active surveillance project beyond the pilot schools to include
additional schools in the pilot states as well as in other states. In
this national rollout, school nurses will continue to receive education
on data collection and ME/CFs as well as technical assistance and
training on using the electronic data collection reporting platform.
This project will extend the currently approved data collection to
involve more school nurses (respondents). This change will help us to
track ME/CFS symptom burden in addition to the ME/CFS prevalence. CDC
requests OMB approval for an estimated 631 annualized burden hours.
There is no cost to respondents other than their time to participate.
(...)
Jeffrey M. Zirger,
Lead, Information Collection Review Office, Office of Public Health
Ethics and Regulations, Office of Science, Centers for Disease Control
and Prevention.
[FR Doc. 2026-02654 Filed 2-10-26; 8:45 am]
BILLING CODE 4163-18-P
Vol. 91, #28, pp 6219-6221
Date: February 11, 2026
URL:
https://www.federalregister.gov/doc...mitted-for-public-comment-and-recommendations
https://www.govinfo.gov/content/pkg/FR-2026-02-11/pdf/2026-02654.pdf
[A Notice by the Centers for Disease Control and Prevention]
Proposed Data Collection Submitted for Public Comment and
Recommendations
-------------------------------------------------------------------------
This document has a comment period that ends in 61 days (04/13/2026)
AGENCY: Centers for Disease Control and Prevention (CDC), Department of
Health and Human Services (HHS).
ACTION: Notice with comment period.
SUMMARY: The Centers for Disease Control and Prevention (CDC), as part
of its continuing effort to reduce public burden and maximize the
utility of government information, invites the general public and other
federal agencies the opportunity to comment on a proposed and/or
continuing information collection, as required by the Paperwork
Reduction Act of 1995. This notice invites comment on a continuing
information collection project titled School-Based Active Surveillance
(SBAS) of Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS)
Among Schoolchildren. This project will expand on the work from previous
phases for active surveillance of chronic conditions, including ME/CFS
and other infection associated chronic conditions and illnesses (IACCs),
using an electronic data collection platform.
DATES: CDC must receive written comments on or before April 13, 2026.
ADDRESSES: You may submit comments, identified by Docket No.
CDC-2026-0166 by either of the following methods:
* Federal eRulemaking Portal: http://www.regulations.gov. Follow the
instructions for submitting comments.
* Mail: Jeffrey M. Zirger, Information Collection Review Office, Centers
for Disease Control and Prevention, 1600 Clifton Road NE, MS H21-8,
Atlanta, Georgia 30329.
Instructions: All submissions received must include the agency name and
Docket Number. CDC will post, without change, all relevant comments to
http://www.regulations.gov.
Please note: Submit all comments through the Federal eRulemaking portal
(http://www.regulations.gov) or by U.S. mail to the address listed
above.
FOR FURTHER INFORMATION CONTACT: To request more information on the
proposed project or to obtain a copy of the information collection plan
and instruments, contact Jeffrey M. Zirger, Information Collection
Review Office, Centers for Disease Control and Prevention, 1600 Clifton
Road NE, MS H21-8, Atlanta, Georgia 30329; Telephone: 404-639-7570;
Email: omb@cdc.gov.
(...)
Background and Brief Description
Myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS), a complex,
chronic, debilitating multi-system disease, affects up to 3.3 million
persons in the United States. However, about 90% of people with ME/CFS
have not received an official diagnosis from a healthcare professional.
ME/CFS affects between 0.10% and 0.75% of children and adolescents,
which often goes undiagnosed by healthcare professionals.
Data on chronic conditions among schoolchildren, such as asthma, has
been collected over the years, but there has been little to no emphasis
on ME/CFS in the United States. Chronic conditions among school-aged
children likely account for a high proportion of chronic school
absenteeism and school withdrawal. Conducting active surveillance among
students using school nurses could expedite the diagnosis and management
of children who present with symptoms commonly seen in ME/CFS. This
involves educating school nurses about ME/CFS and its related syndromes,
how to best approach parents and guardians when suggesting the
diagnosis, and how to support the educational success of students with
chronic diseases.
National active surveillance in schools for ME/CFS coupled with
education of school nurses about ME/CFS could help improve measuring the
burden of ME/CFS in children and provide insights for future plans to
improve healthcare in children suffering from ME/CFS and other chronic
health conditions. In the next phase of this project, we will expand the
active surveillance project beyond the pilot schools to include
additional schools in the pilot states as well as in other states. In
this national rollout, school nurses will continue to receive education
on data collection and ME/CFs as well as technical assistance and
training on using the electronic data collection reporting platform.
This project will extend the currently approved data collection to
involve more school nurses (respondents). This change will help us to
track ME/CFS symptom burden in addition to the ME/CFS prevalence. CDC
requests OMB approval for an estimated 631 annualized burden hours.
There is no cost to respondents other than their time to participate.
(...)
Jeffrey M. Zirger,
Lead, Information Collection Review Office, Office of Public Health
Ethics and Regulations, Office of Science, Centers for Disease Control
and Prevention.
[FR Doc. 2026-02654 Filed 2-10-26; 8:45 am]
BILLING CODE 4163-18-P
bicentennial
Senior Member (Voting Rights)
CDC requests OMB approval for an estimated 631 annualized burden hours.
There is no cost to respondents other than their time to participate. BILLING CODE 4163-18-P
This proposed costing for "burden hours":
- is it for the hours to process feedback from the people concerned about this methodical tightening of an oddly loosened, lax school surveillance, 1995-2026 and ongoing?
- or is it to re-educate many more school nurses, and also brief them on all the symptoms to spot and start recording, keep track of, and add to their numbers of suspected and diagnosed ME/CFS? While it remains the case that 90% is suspected not diagnosed
That is: suspect 90% of 3.3 million people "affected" by ME/CFS. The other 330,000 are diagnosed. So how on earth did anyone get the 3.3m figure?. Are nurses obliged to refer suspected cases, where, for diagnosis?
Its not the highly organised insurance and health providers being tasked to cotton on and produce accurate figures. So much room for error in this data-collection, as formatted.
Is it informed by the WHO, by NICE, by the CDC, and by the Bateman Horne - Cleveland Clinic collaboration etc etc now lodged in the World ME Alliance Education Hub for trusted professionals to inform a world full of clinics and researchers needing info vetted for them?
Where can one review the education of those school nurses in the pilot schools? How was it produced and vetted, when by which parties, and was it outsourced commercially?
How was the ME / CFS community involved in that brand new, co-produced re-education of its own school nurses, or was the educational material just migrated in, from where?
What happened to the easement of training and qualification for school nursing under that 2024 executive order which had it in for nurses? And what was Kennedy Junior's view of that? Oof
Last edited: