nataliezzz
Senior Member (Voting Rights)
*This post is in the process of being updated. People have given me feedback that sharing the Bluesky/Twitter threads is not a preferred/accessible option, so I will try to convey the relevant info here (it will likely have to be spread across multiple threads focusing on sub-topics). This will take time. I'll try to make threads for the different studies/sub-topics slowly over several months.*
Hi everyone,
Some of you may know me from X/Twitter (thanks to those who follow me there, even if you don't directly engage with me it lets me know you see value in what I'm doing/saying )
)
Dr. Avram Gold (medical director of the Stony Brook University Sleep Disorders Center) has proposed a theory that upper airway resistance syndrome (UARS) is a common underlying cause for "chronic complex illnesses" (ME/CFS, fibromyalgia, Gulf War illness, etc.), as well as a causal/contributing factor to many cases of chronic insomnia/anxiety/depression/PTSD. There is no evidence specifically related to UARS and people meeting strict criteria for ME/CFS, but I do think there is enough evidence to assert that UARS is a cause of (at least some cases of) fibromyalgia & Gulf War illness. I'm linking threads I made on the subject on both Bluesky & X/Twitter below (if you don't have an X/Twitter account, you can add "cancel" after the X in the URL to view full threads without an account).
Links to some of the studies mentioned in the threads:
Inspiratory Airflow Dynamics During Sleep in Women with Fibromyalgia
Inspiratory airflow dynamics during sleep in veterans with Gulf War illness: A controlled study
The effect of nasal continuous positive airway pressure on the symptoms of Gulf War illness
Obstructive sleep apnea syndrome as an uncommon cause of fibromyalgia: a case report
Resolution of fibromyalgia by controlling obstructive sleep apnea with a mandibular advancement device
The symptoms and signs of upper airway resistance syndrome: a link to the functional somatic syndromes
Sleep-disordered Breathing and Hypotension
Exploring the Abnormal Modulation of the Autonomic Systems during Nasal Flow Limitation in Upper Airway Resistance Syndrome by Hilbert–Huang Transform
Chronic insomnia (I know ME/CFS/GWI/fibro ≠ chronic insomnia, but many of us have chronic insomnia):
Prospective Randomized Controlled Trial on the Efficacy of Continuous Positive Airway Pressure and Adaptive Servo-Ventilation in the Treatment of Chronic Complex Insomnia
Chronic insomnia remitting after maxillomandibular advancement for mild obstructive sleep apnea: a case series
Prospective Assessment of Nocturnal Awakenings in a Case Series of Treatment-Seeking Chronic Insomnia Patients: A Pilot Study of Subjective and Objective Causes
Upper airway resistance syndrome (UARS) has historically been considered a sleep fragmentation disorder characterized by elevated respiratory effort related arousals (RERAs) + daytime fatigue/sleepiness in the absence of obstructive sleep apnea (OSA), arbitrarily defined as an apnea hypopnea index (AHI) ≥ 5 (obstructive sleep apnea syndrome [OSAS] has also been arbitrarily defined as AHI ≥5 + daytime sleepiness), but UARS appears to be best understood as a stress response disorder driven by sensitization to inspiratory flow limitation (IFL - includes hypopnea, snoring & inaudible "fluttering" of the upper airway due to narrowing/partial collapse during sleep) as a noxious stimulus/stressor. Here is a talk by Dr. Denise Dewald on the physiology/physics of what is occurring in IFL.


Most UARS patients "seek treatment with a somatic functional syndrome rather than sleep-disordered breathing or even a disorder of excessive daytime sleepiness" before eventually being diagnosed with UARS.
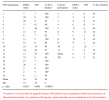
Dr. Gold started with an observation: he noticed alpha-delta sleep (an objective finding well recognized to be associated with fibromyalgia) in many of his UARS patients without a fibromyalgia diagnosis. He also noticed many of his UARS patients complaining of "functional somatic syndrome" symptoms like IBS and body pain. This led him to do small studies of fibromyalgia and Gulf War illness (GWI) patient samples where 27/28 female fibro patients & all 18 male GWI patients had sleep-disordered breathing (SDB)/IFL and they experienced ~35-50% improvement in symptoms (fatigue, pain, sleep quality, etc.) after 3 weeks of CPAP (no control group in the fibro study, but the GWI study had a control group on sham CPAP that did not improve - see details below). One of the fibromyalgia patients who was unemployed due to symptoms and remained on CPAP after the trial returned to full employment.
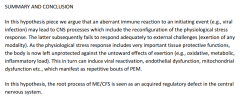
Dr. Gold believes that we had IFL during sleep before we became ill, but our brains did not react to it as a stressor; then HPA axis activation by a stressor (infection, trauma, surgery, chemical/environmental exposure, etc.) sensitized the limbic system to perceive IFL as a noxious stimulus/stressor, and the stress response became ingrained, driving ongoing symptoms. Studies in animal models have demonstrated that activation of the HPA axis by stress can sensitize the limbic system of the brain altering its response to internal and external stimuli (REFERENCES)
Dr. Gold hypothesizes that the sensitization to IFL as a stressor is occurring via the olfactory nerve, which senses nasal airflow/pressure and is directly connected to the limbic system. There is already a known disorder - temporal lobe/limbic epilepsy - for which airflow input to the limbic system via the olfactory nerve is associated with pathological consequences: in patients with temporal lobe/limbic epilepsy, nasal hyperventilation increases the frequency of epileptic EEG abnormalities while oral hyperventilation suppresses them. Locally anesthetizing the olfactory nerve negates the effects of nasal hyperventilation in these individuals.
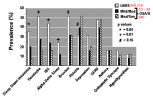
The inverse relationship that has been identified between AHI and the prevalence of "functional somatic syndrome" symptoms like sleep-onset insomnia, headaches and IBS (as well as alpha-delta sleep) in sleep-disordered breathing (SDB) patients could be explained by the fact that as frequency of apneas (complete cessation of airflow) increases, there is less exposure to IFL: "While apnea isolates the nasal airway from the hypopharynx and results in nasal pressure that is equal to atmospheric pressure, hypopnea and, to a greater extent, snoring [or inaudible IFL] lead to prolonged decreases in nasal pressure. Gold postulates that SDB stimulates the HPA axis through the effect of subatmospheric pressure in the nasal airway on the olfactory nerve...the olfactory nerve portion of his paradigm is based on the mechanism by which multiple chemical sensitivity (MCS) is postulated to occur."


This theory could account for many aspects of ME/CFS: how it can be triggered by any kind of stressor, not just infection (I do not buy the suggestion that people with clear non-infectious triggers to their ME/CFS like surgery, childbirth, physical/psychological trauma, chemical exposure, etc. simultaneously acquired an asymptomatic infection which is the real trigger), gradual and rapid onsets, fluctuating severity levels (including fluctuation in symptoms on a daily/hourly basis), remissions and relapses, why people are more likely to recover early on, especially with rest/pacing (stress response less ingrained), and even the "brain retraining" recoveries (for some people, these types of nervous system regulation approaches may be enough to turn off the UARS stress response).
It could also explain why people with hypermobility/EDS are more likely to develop ME/CFS (more lax connective tissue = more collapsible upper airway). A meta-analysis found a 48.9% prevalence of OSA in EDS/Marfan syndrome patients (many more of them could have milder SDB) - on average EDS/Marfan syndrome patients were 6 times more likely than the general population to have OSA.
How might UARS be able to explain PEM? I've linked a detailed Twitter thread on the topic below, but Dr. Herbert Renz-Polster (a doctor with ME/CFS) has considered the nature of PEM (and the objective findings associated with it) in great depth and concluded that PEM is best explained by a dysfunctional central nervous system (CNS) stress response (without knowing anything about UARS, by the way). See his detailed write-up in which he ties in all of the known physiological abnormalities observed in ME/CFS with this hypothesis here:
https://www.kinder-verstehen.de/wp-content/uploads/Mini-Hypothesis-ME.pdf
UARS and obstructive sleep apnea syndrome (OSAS) are not actually separate disorders (at least in many/most cases). It was shown 25 years ago in the first large population-based sleep studies (Sleep Heart Health Study, Wisconsin Sleep Cohort Study) that snoring (which almost always = IFL, though many people have IFL without audible snoring) is the factor most strongly associated with daytime sleepiness, not sleep fragmentation by (apnea/hypopnea/RERA-related) arousals (see links below - these studies only looked at sleepiness and not other symptoms like fatigue and cognitive dysfunction well recognized to be associated with SDB).
Sleep medicine ignored their own data that showed this (persisting with the myth that sleep fragmentation by arousals is the primary cause of sleepiness/fatigue/cognitive dysfunction in sleep-disordered breathing patients), and thanks to that we have ended up in the situation we are now with millions of sleep-disordered breathing patients being deprived of appropriate treatment simply because they have an AHI <5 (insurance generally doesn't cover CPAP and other treatments for people with an AHI <5). It's kind of mind boggling how long this disaster has gone on for, considering how easily the sleep fragmentation paradigm of sleep-disordered breathing falls apart: if sleep fragmentation were the primary cause of symptoms in sleep-disordered breathing patients, why would we have OSA vs. OSA syndrome & >50% of people with OSA being asymptomatic?
Relation of Sleepiness to Respiratory Disturbance Index The Sleep Heart Health Study
The Occurrence of Sleep-Disordered Breathing among Middle-Aged Adults
Does Snoring Predict Sleepiness Independently of Apnea and Hypopnea Frequency?
Bluesky thread I made summarizing the data from the above studies
Here is another study that supports the importance of inspiratory flow limitation in the symptomatology of SDB patients; in 998 suspected OSA patients referred for polysomnography, increased flow limitation frequency was associated with increased psychomotor vigilance task (PVT) lapses; AHI was not.
Increased Flow Limitation During Sleep Is Associated With Increased Psychomotor Vigilance Task Lapses in Individuals With Suspected OSA
So how could we have a person with high blood pressure and a primary complaint of sleepiness (our classic OSAS patient) and a person with low blood pressure/orthostatic intolerance with a primary complaint of fatigue actually having (differing presentations of) the same underlying disorder? I think the reasons there are such hugely varying presentations of UARS/OSAS are:
1) People's brains/bodies react very differently to the stress IFL induces; some may have sleepiness > fatigue while others have fatigue > sleepiness, for some the primary complaint may be body pain/insomnia/headaches/IBS/etc. without dramatic fatigue or sleepiness. I just see ME/CFS as the most severe presentation of UARS (& many of us, myself included, had milder symptoms/issues [e.g. cold hands/feet without overt OI in my case] that were likely caused by UARS before we developed full-blown ME/CFS). Also many of us (myself included) who had a clearly defined rapid onset to our ME/CFS, did not have PEM (the pathognomonic symptom of ME/CFS) when our symptoms began and only developed it later into the illness course (I highly doubt that I developed a different disorder when PEM emerged in addition to the fatigue and unrefreshing sleep I was previously experiencing). If UARS is indeed causing ME/CFS, I suspect that many of us likely have both:
Gulf War illness study (1, 2):
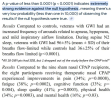
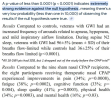
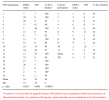
18 GWI patients had 96%±5 of their breaths flow limited while 11 age/BMI-matched asymptomatic Gulf War vets had 36±25% of their breaths flow limited (p <.0001). The GWI patients treated with therapeutic CPAP experienced improvements in the symptoms of GWI (fatigue, pain, cognitive dysfunction, etc.) which were significantly correlated with changes in an objective finding (decreased sleep stage shifts) in all patients (GWI patients on sham CPAP did not experience decreased sleep stage shifts & got slightly worse).

Linking towards the end of the thread as it is long & it doesn't automatically unroll the whole thing:
Thread continued here; includes my own ME/CFS story and improvements with treating my UARS. I made this account on X to help raise awareness of PSSD (post-SSRI sexual dysfunction); I probably should have made a new account for the UARS stuff back when I first started talking about it - oh well lol.
Thread with more info on the UARS/OSAS - fibromyalgia connection, including 2 case reports of dramatic resolution of fibromyalgia symptoms from treating OSA. I think there was enough evidence to say UARS/OSAS could cause fibromyalgia without these, but they seal the deal (esp. because they are not coming from Dr. Gold); alpha-delta sleep is an objective finding associated with fibromyalgia (& UARS) and if it disappears along with fibromyalgia symptoms with treatment of UARS/OSAS, I think it's fair to conclude that UARS/OSAS is the cause of (that person's) fibromyalgia
Thread on why I think UARS can explain PEM & why I think PEM is best explained as a CNS problem (including discussion of how benzodiazepines alleviate/reduce PEM symptoms for many patients, as well as prevent/reduce PEM when taken ahead of exertion - and the same is true for other CNS depressants/sedatives like dextromethorphan):
https://x.com/PSSD_Info/status/1924352017792737568
Thread on why I think CPAP/BiPAP is not typically a cure for ME/CFS/fibro/etc. patients (basically, it also seems to be acting as a stressor on a sensitized nervous system).
Also, to help put some of the findings of the studies in my thread in context:
https://pmc.ncbi.nlm.nih.gov/articles/PMC4561280/ Prevalence of OSA (AHI ≥5) in the general population in 11 published epidemiological studies: mean of 22% (range, 9-37%) in men and 17% (range, 4-50%) in women. Some studies oversampled habitual snorers.
https://www.sciencedirect.com/science/article/abs/pii/S1389945722000478 Attempted UARS prevalence study from the São Paulo Epidemiologic Sleep Study data found a 3.1% prevalence with 4.4% in females and 1.5% in males (UARS criteria was IFL time ≥5% of total sleep time, minimum SpO2 ≥92%, AHI < 5, and symptoms of excessive daytime sleepiness or fatigue) - I am not sure if people with diagnoses like ME/CFS were excluded as I couldn't access the full paper.
I look forward to (hopefully) hearing from people and getting the conversation started.
-Natalie
Hi everyone,
Some of you may know me from X/Twitter (thanks to those who follow me there, even if you don't directly engage with me it lets me know you see value in what I'm doing/saying
Dr. Avram Gold (medical director of the Stony Brook University Sleep Disorders Center) has proposed a theory that upper airway resistance syndrome (UARS) is a common underlying cause for "chronic complex illnesses" (ME/CFS, fibromyalgia, Gulf War illness, etc.), as well as a causal/contributing factor to many cases of chronic insomnia/anxiety/depression/PTSD. There is no evidence specifically related to UARS and people meeting strict criteria for ME/CFS, but I do think there is enough evidence to assert that UARS is a cause of (at least some cases of) fibromyalgia & Gulf War illness. I'm linking threads I made on the subject on both Bluesky & X/Twitter below (if you don't have an X/Twitter account, you can add "cancel" after the X in the URL to view full threads without an account).
Links to some of the studies mentioned in the threads:
Inspiratory Airflow Dynamics During Sleep in Women with Fibromyalgia
Inspiratory airflow dynamics during sleep in veterans with Gulf War illness: A controlled study
The effect of nasal continuous positive airway pressure on the symptoms of Gulf War illness
Obstructive sleep apnea syndrome as an uncommon cause of fibromyalgia: a case report
Resolution of fibromyalgia by controlling obstructive sleep apnea with a mandibular advancement device
The symptoms and signs of upper airway resistance syndrome: a link to the functional somatic syndromes
Sleep-disordered Breathing and Hypotension
Exploring the Abnormal Modulation of the Autonomic Systems during Nasal Flow Limitation in Upper Airway Resistance Syndrome by Hilbert–Huang Transform
Chronic insomnia (I know ME/CFS/GWI/fibro ≠ chronic insomnia, but many of us have chronic insomnia):
Prospective Randomized Controlled Trial on the Efficacy of Continuous Positive Airway Pressure and Adaptive Servo-Ventilation in the Treatment of Chronic Complex Insomnia
Chronic insomnia remitting after maxillomandibular advancement for mild obstructive sleep apnea: a case series
Prospective Assessment of Nocturnal Awakenings in a Case Series of Treatment-Seeking Chronic Insomnia Patients: A Pilot Study of Subjective and Objective Causes
Upper airway resistance syndrome (UARS) has historically been considered a sleep fragmentation disorder characterized by elevated respiratory effort related arousals (RERAs) + daytime fatigue/sleepiness in the absence of obstructive sleep apnea (OSA), arbitrarily defined as an apnea hypopnea index (AHI) ≥ 5 (obstructive sleep apnea syndrome [OSAS] has also been arbitrarily defined as AHI ≥5 + daytime sleepiness), but UARS appears to be best understood as a stress response disorder driven by sensitization to inspiratory flow limitation (IFL - includes hypopnea, snoring & inaudible "fluttering" of the upper airway due to narrowing/partial collapse during sleep) as a noxious stimulus/stressor. Here is a talk by Dr. Denise Dewald on the physiology/physics of what is occurring in IFL.


Most UARS patients "seek treatment with a somatic functional syndrome rather than sleep-disordered breathing or even a disorder of excessive daytime sleepiness" before eventually being diagnosed with UARS.
Dr. Gold started with an observation: he noticed alpha-delta sleep (an objective finding well recognized to be associated with fibromyalgia) in many of his UARS patients without a fibromyalgia diagnosis. He also noticed many of his UARS patients complaining of "functional somatic syndrome" symptoms like IBS and body pain. This led him to do small studies of fibromyalgia and Gulf War illness (GWI) patient samples where 27/28 female fibro patients & all 18 male GWI patients had sleep-disordered breathing (SDB)/IFL and they experienced ~35-50% improvement in symptoms (fatigue, pain, sleep quality, etc.) after 3 weeks of CPAP (no control group in the fibro study, but the GWI study had a control group on sham CPAP that did not improve - see details below). One of the fibromyalgia patients who was unemployed due to symptoms and remained on CPAP after the trial returned to full employment.
Dr. Gold believes that we had IFL during sleep before we became ill, but our brains did not react to it as a stressor; then HPA axis activation by a stressor (infection, trauma, surgery, chemical/environmental exposure, etc.) sensitized the limbic system to perceive IFL as a noxious stimulus/stressor, and the stress response became ingrained, driving ongoing symptoms. Studies in animal models have demonstrated that activation of the HPA axis by stress can sensitize the limbic system of the brain altering its response to internal and external stimuli (REFERENCES)
Dr. Gold hypothesizes that the sensitization to IFL as a stressor is occurring via the olfactory nerve, which senses nasal airflow/pressure and is directly connected to the limbic system. There is already a known disorder - temporal lobe/limbic epilepsy - for which airflow input to the limbic system via the olfactory nerve is associated with pathological consequences: in patients with temporal lobe/limbic epilepsy, nasal hyperventilation increases the frequency of epileptic EEG abnormalities while oral hyperventilation suppresses them. Locally anesthetizing the olfactory nerve negates the effects of nasal hyperventilation in these individuals.
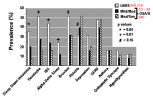
The inverse relationship that has been identified between AHI and the prevalence of "functional somatic syndrome" symptoms like sleep-onset insomnia, headaches and IBS (as well as alpha-delta sleep) in sleep-disordered breathing (SDB) patients could be explained by the fact that as frequency of apneas (complete cessation of airflow) increases, there is less exposure to IFL: "While apnea isolates the nasal airway from the hypopharynx and results in nasal pressure that is equal to atmospheric pressure, hypopnea and, to a greater extent, snoring [or inaudible IFL] lead to prolonged decreases in nasal pressure. Gold postulates that SDB stimulates the HPA axis through the effect of subatmospheric pressure in the nasal airway on the olfactory nerve...the olfactory nerve portion of his paradigm is based on the mechanism by which multiple chemical sensitivity (MCS) is postulated to occur."


This theory could account for many aspects of ME/CFS: how it can be triggered by any kind of stressor, not just infection (I do not buy the suggestion that people with clear non-infectious triggers to their ME/CFS like surgery, childbirth, physical/psychological trauma, chemical exposure, etc. simultaneously acquired an asymptomatic infection which is the real trigger), gradual and rapid onsets, fluctuating severity levels (including fluctuation in symptoms on a daily/hourly basis), remissions and relapses, why people are more likely to recover early on, especially with rest/pacing (stress response less ingrained), and even the "brain retraining" recoveries (for some people, these types of nervous system regulation approaches may be enough to turn off the UARS stress response).
It could also explain why people with hypermobility/EDS are more likely to develop ME/CFS (more lax connective tissue = more collapsible upper airway). A meta-analysis found a 48.9% prevalence of OSA in EDS/Marfan syndrome patients (many more of them could have milder SDB) - on average EDS/Marfan syndrome patients were 6 times more likely than the general population to have OSA.
How might UARS be able to explain PEM? I've linked a detailed Twitter thread on the topic below, but Dr. Herbert Renz-Polster (a doctor with ME/CFS) has considered the nature of PEM (and the objective findings associated with it) in great depth and concluded that PEM is best explained by a dysfunctional central nervous system (CNS) stress response (without knowing anything about UARS, by the way). See his detailed write-up in which he ties in all of the known physiological abnormalities observed in ME/CFS with this hypothesis here:
https://www.kinder-verstehen.de/wp-content/uploads/Mini-Hypothesis-ME.pdf
UARS and obstructive sleep apnea syndrome (OSAS) are not actually separate disorders (at least in many/most cases). It was shown 25 years ago in the first large population-based sleep studies (Sleep Heart Health Study, Wisconsin Sleep Cohort Study) that snoring (which almost always = IFL, though many people have IFL without audible snoring) is the factor most strongly associated with daytime sleepiness, not sleep fragmentation by (apnea/hypopnea/RERA-related) arousals (see links below - these studies only looked at sleepiness and not other symptoms like fatigue and cognitive dysfunction well recognized to be associated with SDB).
Sleep medicine ignored their own data that showed this (persisting with the myth that sleep fragmentation by arousals is the primary cause of sleepiness/fatigue/cognitive dysfunction in sleep-disordered breathing patients), and thanks to that we have ended up in the situation we are now with millions of sleep-disordered breathing patients being deprived of appropriate treatment simply because they have an AHI <5 (insurance generally doesn't cover CPAP and other treatments for people with an AHI <5). It's kind of mind boggling how long this disaster has gone on for, considering how easily the sleep fragmentation paradigm of sleep-disordered breathing falls apart: if sleep fragmentation were the primary cause of symptoms in sleep-disordered breathing patients, why would we have OSA vs. OSA syndrome & >50% of people with OSA being asymptomatic?
Relation of Sleepiness to Respiratory Disturbance Index The Sleep Heart Health Study
The Occurrence of Sleep-Disordered Breathing among Middle-Aged Adults
Does Snoring Predict Sleepiness Independently of Apnea and Hypopnea Frequency?
Bluesky thread I made summarizing the data from the above studies
Here is another study that supports the importance of inspiratory flow limitation in the symptomatology of SDB patients; in 998 suspected OSA patients referred for polysomnography, increased flow limitation frequency was associated with increased psychomotor vigilance task (PVT) lapses; AHI was not.
Increased Flow Limitation During Sleep Is Associated With Increased Psychomotor Vigilance Task Lapses in Individuals With Suspected OSA
So how could we have a person with high blood pressure and a primary complaint of sleepiness (our classic OSAS patient) and a person with low blood pressure/orthostatic intolerance with a primary complaint of fatigue actually having (differing presentations of) the same underlying disorder? I think the reasons there are such hugely varying presentations of UARS/OSAS are:
1) People's brains/bodies react very differently to the stress IFL induces; some may have sleepiness > fatigue while others have fatigue > sleepiness, for some the primary complaint may be body pain/insomnia/headaches/IBS/etc. without dramatic fatigue or sleepiness. I just see ME/CFS as the most severe presentation of UARS (& many of us, myself included, had milder symptoms/issues [e.g. cold hands/feet without overt OI in my case] that were likely caused by UARS before we developed full-blown ME/CFS). Also many of us (myself included) who had a clearly defined rapid onset to our ME/CFS, did not have PEM (the pathognomonic symptom of ME/CFS) when our symptoms began and only developed it later into the illness course (I highly doubt that I developed a different disorder when PEM emerged in addition to the fatigue and unrefreshing sleep I was previously experiencing). If UARS is indeed causing ME/CFS, I suspect that many of us likely have both:
- Mild sleep-disordered breathing (high % IFL with little/no time spent in apnea to balance it out)
- Highly sensitized to IFL
Gulf War illness study (1, 2):
18 GWI patients had 96%±5 of their breaths flow limited while 11 age/BMI-matched asymptomatic Gulf War vets had 36±25% of their breaths flow limited (p <.0001). The GWI patients treated with therapeutic CPAP experienced improvements in the symptoms of GWI (fatigue, pain, cognitive dysfunction, etc.) which were significantly correlated with changes in an objective finding (decreased sleep stage shifts) in all patients (GWI patients on sham CPAP did not experience decreased sleep stage shifts & got slightly worse).

Linking towards the end of the thread as it is long & it doesn't automatically unroll the whole thing:
Thread continued here; includes my own ME/CFS story and improvements with treating my UARS. I made this account on X to help raise awareness of PSSD (post-SSRI sexual dysfunction); I probably should have made a new account for the UARS stuff back when I first started talking about it - oh well lol.
Thread with more info on the UARS/OSAS - fibromyalgia connection, including 2 case reports of dramatic resolution of fibromyalgia symptoms from treating OSA. I think there was enough evidence to say UARS/OSAS could cause fibromyalgia without these, but they seal the deal (esp. because they are not coming from Dr. Gold); alpha-delta sleep is an objective finding associated with fibromyalgia (& UARS) and if it disappears along with fibromyalgia symptoms with treatment of UARS/OSAS, I think it's fair to conclude that UARS/OSAS is the cause of (that person's) fibromyalgia
Thread on why I think UARS can explain PEM & why I think PEM is best explained as a CNS problem (including discussion of how benzodiazepines alleviate/reduce PEM symptoms for many patients, as well as prevent/reduce PEM when taken ahead of exertion - and the same is true for other CNS depressants/sedatives like dextromethorphan):
https://x.com/PSSD_Info/status/1924352017792737568
Thread on why I think CPAP/BiPAP is not typically a cure for ME/CFS/fibro/etc. patients (basically, it also seems to be acting as a stressor on a sensitized nervous system).
Also, to help put some of the findings of the studies in my thread in context:
https://pmc.ncbi.nlm.nih.gov/articles/PMC4561280/ Prevalence of OSA (AHI ≥5) in the general population in 11 published epidemiological studies: mean of 22% (range, 9-37%) in men and 17% (range, 4-50%) in women. Some studies oversampled habitual snorers.
https://www.sciencedirect.com/science/article/abs/pii/S1389945722000478 Attempted UARS prevalence study from the São Paulo Epidemiologic Sleep Study data found a 3.1% prevalence with 4.4% in females and 1.5% in males (UARS criteria was IFL time ≥5% of total sleep time, minimum SpO2 ≥92%, AHI < 5, and symptoms of excessive daytime sleepiness or fatigue) - I am not sure if people with diagnoses like ME/CFS were excluded as I couldn't access the full paper.
I look forward to (hopefully) hearing from people and getting the conversation started.
-Natalie
Last edited: