Fibromyalgia and ICD-11 coding - Editorial, published June 2022
As I've mentioned several times before in this thread, the relocation of FM to the
Symptoms, signs chapter was effected in the ICD-11 Beta draft in May 2015
without proposals to do so having first been submitted via the ICD-11 Beta draft Proposal Platform for clinical and public scrutiny and comment.
A number of advocates associated with FM patients groups were alerted to this change of chapter location several years ago and were more recently advised via Twitter threads how to submit patient org comments to the Proposal Platform. None of them appeared to have taken this forward.
[Paragraphs inserted for ease of reading]
June 202
Clinical and Experimental Rheumatology 40(6)
Editorial
Concerns about the taxonomy, definition and codingof fibromyalgia syndrome in ICD-11: the potentialfor negative consequences for patient care and research
W. Häuser1, D.J. Clauw2, F. Wolfe3, P. Sarzi-Puttini4, J.N. Ablin5, C. Usui6,G.O. Littlejohn7, B. Morlion8, E. Kosek9,10, E.A. Fors11, K.M. Øien Forseth12,M.-A. Fitzcharles13,14
DOI: http://dx.doi.org/10.55563/clinexprheumatol/3bt9qx
Full text available for free from:
Abstract: https://www.clinexprheumatol.org/abstract.asp?a=18721
PDF: https://www.clinexprheumatol.org/article.asp?a=18721
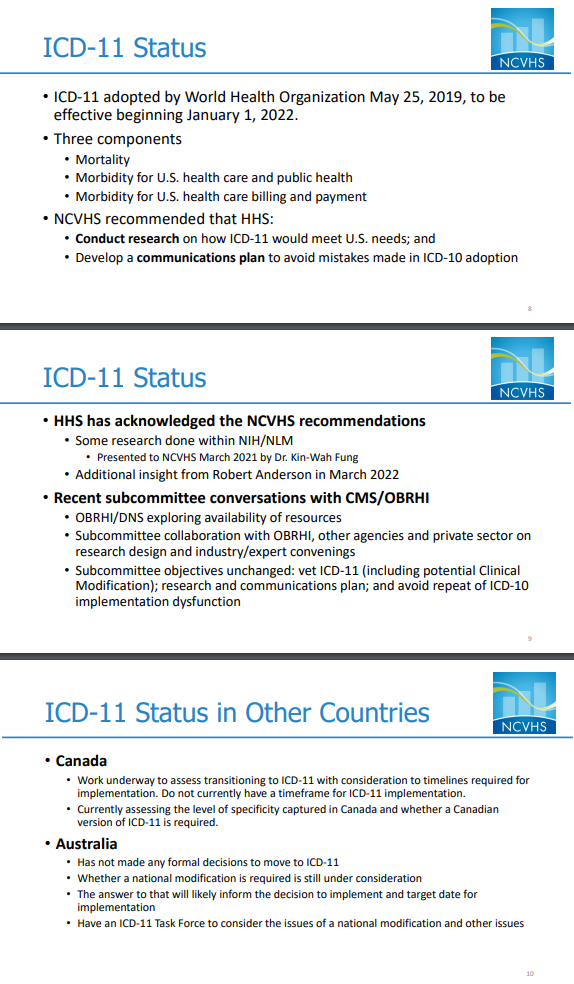
International Statistical Classification of Diseases and Related Health Problems (ICD) codes of the World Health Organisation (WHO) are currently used by about 27 countries worldwide, primarily for reimbursement and resource allocation, but have become an important source of health care services research. The current ICD-10 was replaced by ICD-11 on January 1, 2022. An important change introduced in the ICD-11 is the systematic classification of clinical conditions associated with chronic pain (1), as proposed by an interdisciplinary working group of the International Association of the Study of Pain (IASP) and the WHO (2, 3).
Fibromyalgia syndrome (FMS) was relocated from its legacy ICD-10 chapter location (diseases of the musculoskeletal system and connective tissue) to the new category block in the chapter “Symptoms, signs or clinical findings, not elsewhere classified”, as an inclusion term under Chronic primary pain > Chronic widespread pain (CWP).
This working group did not discuss the new definition and classification of FMS in the ICD-11 with the boards of other medical associations (e.g. rheumatology) or FMS-patient organisations.
As clinicians, researchers and guideline makers occupied with FMS, we offer critical comment on taxonomy, definition and coding of FMS according to the ICD-11 and the potential for negative consequences for patient care and research.
Taxonomy
FMS is no longer identified as a condition of the musculoskeletal system, contrary to current understanding in the literature (4). Remarkably, the body structures involved in CWP as listed in the IASP proposal of June 26, 2019, namely connective tissue, skeletal and/or smooth muscle structures (5) have been eliminated in the ICD-11.
The IASP working group has not published any statement to provide clarification of why the initial proposal with which we agree has not been incorporated into the definition of CWP and FMS in ICD-11. The five body quadrants identified for pain location for CWP and FM include (upper left, upper right, lower left, lower right of the body) and axial (neck, back, chest and abdomen) (1-3). With the ICD-11 requirement that 4 of 5 body regions be painful in order to meet FMS criteria, primary headache and irritable bowel syndrome (IBS) pain could be attributed to FMS. Thus, the ICD-11 definition of FMS has transformed FMS to be a multisystem pain disorder. We acknowledge that many FMS-patients meet the criteria of other chronic pain syndromes such as irritable bowel syndrome or chronic tension headache (so-called overlapping pain conditions) (6). However, this statement similarly also applies to other chronic primary pain conditions (7). The consideration of potential comorbidities is important for the management of FMS (8). However, a “lumping” approach including different chronic pain syndromes such as FMS, IBS and chronic tension headache in one category is not appropriate because – besides common general treatment principles such as education and physical activity – specific pharmacological treatment options are recommended for each of these chronic primary pain syndromes and may differ according to the condition.
Chronic primary headaches are crossreferenced in this section making use of the “multiple parenting” option of ICD-11, which means that chronic migraine is listed in both the headache section and the chronic pain section (2). We suggest that “multiple parenting” should also be possible for FMS in ICD-11. We believe that FMS should receive a diagnostic code in the chapter “Diseases of the musculoskeletal system or connective tissue”, too.
In addition, we suggest that FMS should be integrated in the subcategory “chronic primary musculoskeletal pain” as “chronic primary widespread musculoskeletal pain” (9) in accordance with the meaning and understanding of fibromyalgia (pain in muscles and tendons) and its current use in the literature (4). Moreover, we suggest that pain sites in the head, face, and abdomen should be excluded in the definition of FM as outlined by the 2016 criteria (10).
(...)
Coding
(...)
We express our concerns that the lack of a unique code for FMS has the potential for negative consequences for patient care. There remain many health care providers claiming that FMS does not exist (15).
Legitimacy of FMS as a disease was previously supported when the WHO assigned a unique diagnostic code in ICD-9 and ICD-10. Thus, ICD-11 is retrogressive compared to ICD-9 and ICD-10. In addition, the lack of a unique diagnostic code for FMS can compromise patient care and research. In countries, where ICD code use is obligatory, treatment reimbursement may be challenging. Finally, health care services with data of statutory health insurance companies in countries which require ICD-codes will no longer be possible.
We suggest that a unique diagnostic code be assigned to FMS which is different from that of CWP.
We understand that the final ICD-11 classification was a compromise within the IASP/WHO working group between divergent opinions regarding the elimination or retention of a diagnostic code for FMS (R.-D. Treede, personal communication). It is unfortunate that these imminent changes in the ICD-11 were not more widely discussed in the pain or rheumatology communities nor with FMS patient representatives.
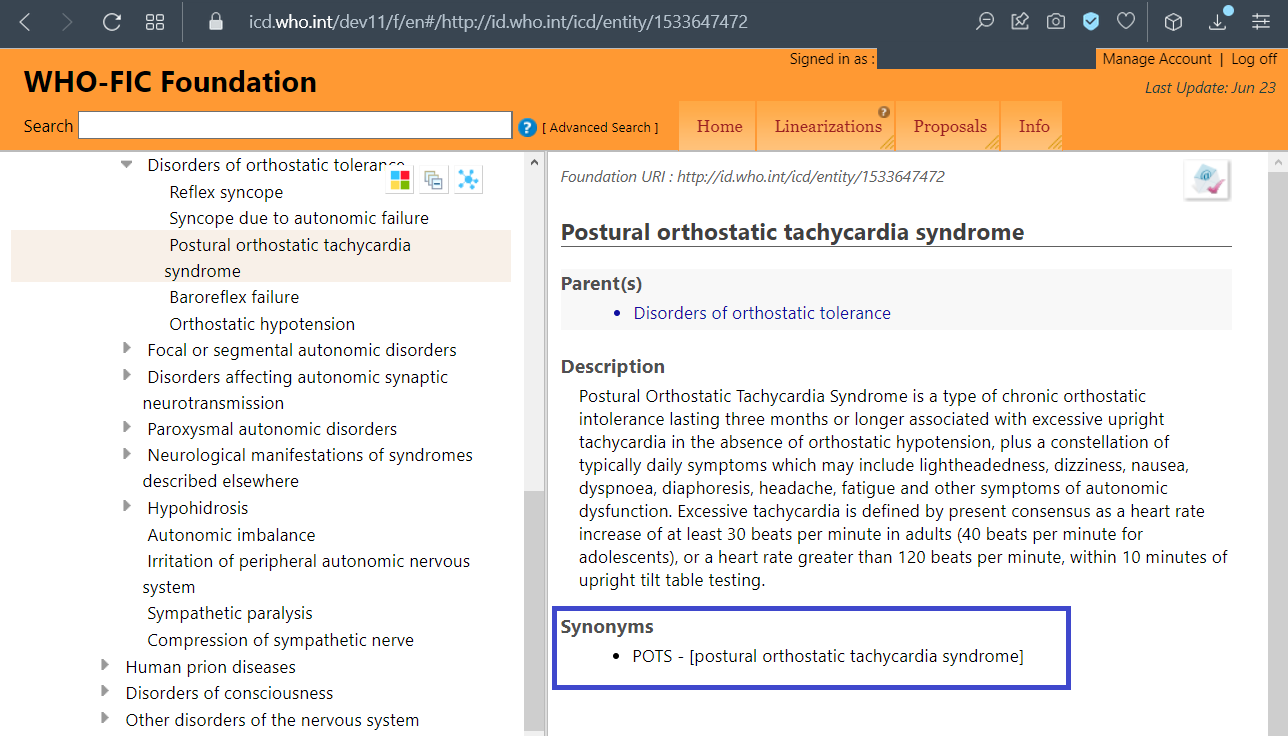
The WHO offers a webpage for comments on the ICD-11:
https://icd.who.int/dev11. If the reader of this paper, patient organisations and medical associations share (some of) our concerns and suggestions, we urge that commentary could be made on this webpage. We hope that sufficient comment will prompt the IASP/WHO working group to modify the taxonomy, definition and coding of FMS in ICD-11.
Full free text attached to this post or can be downloaded from:
Abstract: https://www.clinexprheumatol.org/abstract.asp?a=18721
PDF: https://www.clinexprheumatol.org/article.asp?a=18721
[Edit: Corrected "May 2016" to May 2015.]