The next meeting of the NCHS/CDC ICD-10-CM Coordination and Maintenance Committee takes place on Tuesday and Wednesday this coming week (14-15 September):
https://www.cdc.gov/nchs/icd/icd10cm_maintenance.htm
The Final Agenda (Diagnosis Codes Topic Packet) is now available:
https://www.cdc.gov/nchs/icd/Sept2021-TopicPacket.pdf
NB: Proposals for changes to the US's ICD-10-CM Tabular List and Index were submitted by SOLVE ME, supported by six US organisations, including IACFS/ME and #MEAction.
The proposals, as set out in the Final Agenda, have been modified by NCHS and are not the same as the proposals submitted last December by SOLVE ME et al.
These proposals relate only to the US's ICD-10-CM, which was developed by NCHS/CDC, and is managed, revised and updated by NCHS/CDC - not by the WHO.
These proposals do not relate to the WHO's International edition of ICD-10; to ICD-11 or to any of the various national modifications of ICD-10.
The proposals are scheduled for discussion at the NCHS/CDC C & M public meeting, this coming week (Tuesday 14 and Wednesday 15 September), which will be held virtually. CDC may potentially present alternative proposals at the meeting which have not been included in the Final Agenda (Topic Packet).
No decisions on proposals are made at the meeting, itself. Following the meeting, there will be a public review and feedback period during which comment, objections etc can be submitted to NCHS/CDC.
The Final Agenda (Diagnosis Codes Topic Packet) is here:
https://www.cdc.gov/nchs/icd/Sept2021-TopicPacket.pdf
The agenda topic:
Postviral and Related Fatigue Syndromes
Traci Ramirez (Ed: CDC)
Mary Dimmock
is listed on Page 169 of what looks to be a very full agenda. This will be a virtual meeting and presentation and discussion of the diagnosis code proposals may run on into Day Two.
Extract Page 169:
https://www.cdc.gov/nchs/icd/Sept2021-TopicPacket.pdf
Rationale for proposal submitted by SOLVE ME:
Postviral and Related Fatigue Syndromes
In 2015, the Institute of Medicine (IOM), now called the National Academy of Medicine, published an extensive evidence review of “myalgic encephalomyelitis/chronic fatigue syndrome” (ME/CFS) and recommended new diagnostic criteria. The CDC, disease experts, and many clinical guidance and medical education providers have already adopted the IOM criteria along with the term “myalgic encephalomyelitis/chronic fatigue syndrome.” Postviral Fatigue Syndrome proposals were presented at the September 2011 and September 2018 C&M meetings; the comments did not support the proposals. An updated proposal is included. This new proposal was submitted by The International Association for Chronic Fatigue Syndrome/Myalgic Encephalomyelitis, #MEAction, Open Medicine Foundation, Solve M.E., Massachusetts ME/CFS & FM Association, the Minnesota ME/CFS Alliance, and Pandora Org.
Currently, the term does not exist in the ICD-10-CM and the ICD-10-CM code most often used is the one for “chronic fatigue syndrome,” which is the same code as the symptom of “chronic fatigue”, (R53.82). As a result, it is difficult to accurately track ME/CFS separate from the symptom of chronic fatigue. This could also have secondary effects on healthcare resource planning, fiscal support for clinical care, use of medical records in future research, provisioning of workplace/school accommodations, and determination of disability benefits.
In its 2015 report, the Institute of Medicine concluded that ME/CFS is “a serious, chronic, complex, and multisystem disease,” characterized by the hallmark symptom of post-exertional malaise (PEM) in which even small amounts of cognitive and physical exertion can exacerbate symptoms that can last for days, weeks or sometimes months. ME/CFS is debilitating with an estimated 25% of patients homebound or bedbound and as many as 75% unable to work or go to school. ME/CFS is known to often follow a viral infection
The rationale for including ME/CFS as a synonym to ME is that the ME and ME/CFS criteria, including the IOM criteria, all require the hallmark symptoms of post-exertional malaise, unrefreshing sleep, profound fatigue, and significant impairment in function. These criteria also include other symptoms such as cognitive impairment, orthostatic intolerance, pain, and sensory sensitivity. The US ME/CFS Clinician Coalition recommends the IOM criteria for diagnosis in the US, but also acknowledges the similarities across these definitions and notes that some experts use the 2003 Canadian Consensus Criteria (labeled as ME/CFS) and the 2011 ME International Consensus Criteria (labeled as ME) to validate an IOM-criteria clinical diagnosis of ME/CFS.
The IOM report established new diagnostic criteria that include PEM and substantial impairment in functioning, profound fatigue, unrefreshing sleep, and either cognitive issues or orthostatic intolerance. Other common but non-required symptoms include joint and muscle pain, headaches, and sensitivity to noise and light. Published peer-reviewed studies have demonstrated neurological, immunological, autonomic, and energy metabolism impairment associated with these symptoms.
In addition to the new clinical diagnostic criteria, the IOM also recommended a new name, “Systemic exertion intolerance disease (SEID).” Federal agencies including CDC and NIH, disease experts, and medical education and clinical guidance providers have adopted the term “ME/CFS,” instead of SEID, along with the new clinical diagnostic criteria recommended by the IOM in the 2015 report.
The IOM noted that not all persons previously diagnosed with CFS using the Fukuda CFS definition, used in the US prior to adoption of the IOM criteria, would meet the new IOM criteria for ME/CFS. The IOM did not intend the term ME/CFS to be a replacement for the term chronic fatigue syndrome or an amalgamation of all ME and CFS diagnoses.
Consideration was given as a potential alternative is to have coders separately apply the two codes for the terms, myalgic encephalomyelitis and chronic fatigue syndrome when the doctor diagnoses ME/CFS. However, this does not capture the name of the disease as specified by the doctor or in clinical guidance and medical education. Additionally, this currently could not be done due to existing instructional (Excludes1) notes.
The code title for ICD-10-CM code, G93.3, is currently, postviral fatigue syndrome (PVFS) and ME is an inclusion term. Because the G93.3 title specifies postviral illness, some doctors have declined to diagnose ME when viral illness is not proven. However, according to practice and established criteria, ME can be triggered by both viral and non-viral precipitants, including nonviral infections and non-infectious causes. This is also true for the definitions that use the ME/CFS label, including the IOM criteria.
It is also being recommended the code title G93.3, Postviral fatigue syndrome, be revised to Postviral and related fatigue syndromes to include other precipitants and still maintain the code title’s original wording. By its name, the term postviral fatigue syndrome is intended only for post-viral illness.
But as noted above, the terms ME and ME/CFS include both viral and nonviral precipitants. The ME and ME/CFS definitions further specify that symptoms should persist for 6 months while PVFS is used even if patients have not been sick for six months.
References
1. Institute of Medicine. Beyond Myalgic Encephalomyelitis/Chronic Fatigue Syndrome: Redefining an Illness. The National Academies Press; May 2015.
https://www.nap.edu/catalog/19012/b...chronic-fatiguesyndrome-redefining-an-illness
2. In addition to the US ME/CFS Clinician Coalition, examples of medical education and clinical guidance providers that use the ME/CFS term and the IOM criteria include
• CDC ME/CFS website –
https://www.cdc.gov/me-cfs/index.html
• Medscape 2019 ME/CFS CME -
https://www.medscape.org/viewarticle/907632?src=acdmpart_cdc
• Kaiser Permanente. ME/CFS medical information.
https://healthy.kaiserpermanente.or...halomyelitis-chronic-fatigue-syndrome.hw32907 Content provided by Healthwise which provides content to a number of other sites as well
• Cleveland Clinic -
https://my.clevelandclinic.org/heal...ncephalomyelitischronic-fatiguesyndrome-mecfs
3. US ME/CFS Clinician Coalition letter to medical providers. October 30, 2020
Code:
https://drive.google.com/file/d/15Z1pPMsTvxKe_eJtNG3XyXNxx9gB2xxU/view
4. US ME/CFS Clinician Coalition Handout. July 2020.
Code:
https://drive.google.com/file/d/1SG7hlJTCSDrDHqvioPMq-cX-rgRKXjfk/view
5. Bateman L, et al. Myalgic Encephalomyelitis/Chronic Fatigue Syndrome: Essentials of Diagnosis and Management Mayo Clinic Proceedings. August 2021.
https://www.mayoclinicproceedings.org/article/S0025-6196(21)00513-9/fulltext
6. ICD-10-CM Official Guidelines for Coding and Reporting. FY2020
https://www.cdc.gov/nchs/data/icd/10cmguidelines-FY2020_final.pdf
7. Institute of Medicine 2015 report. Page 210.
8. Institute of Medicine 2015 report. Page 1. Also see the 2003 Canadian Consensus Criteria and the 2011 ME International Criteria which use the terms ME/CFS and ME respectively.
• Carruthers B, Jain A, De Meirleir K, Peterson D, Klimas N, et al. Myalgic encephalomyelitis/chronic fatigue syndrome: Clinical working case definition, diagnostic and treatment protocols (Canadian case definition). Journal of Chronic Fatigue Syndrome. 2003 11(1):7-115.
• Carruthers B. van de Sande M, De Meirleir K, Klimas N, Broderick G, et al. Myalgic encephalomyelitis: International consensus criteria. Journal of Internal Medicine 2011. 270(4):327-338.
9. World Health Organization ICD-10: Version 2019.
https://icd.who.int/browse10/2019/en#/F48.0
10. International Association of CFS/ME Chronic fatigue syndrome/myalgic encephalomyelitis Primer for Clinical Practitioners Primer. 2014.
https://growthzonesitesprod.azureed.../1869/2020/10/Primer_Post_2014_conference.pdf
11. Institute of Medicine 2015 report. Page 5
12. Institute of Medicine 2015 report. Page 8, 77
13. See the evidence review in the Institute of Medicine report. Also see Komaroff AL. Advances in understanding the pathophysiology of chronic fatigue syndrome. JAMA. 2019;322(6):499.
[Proposal text ends]
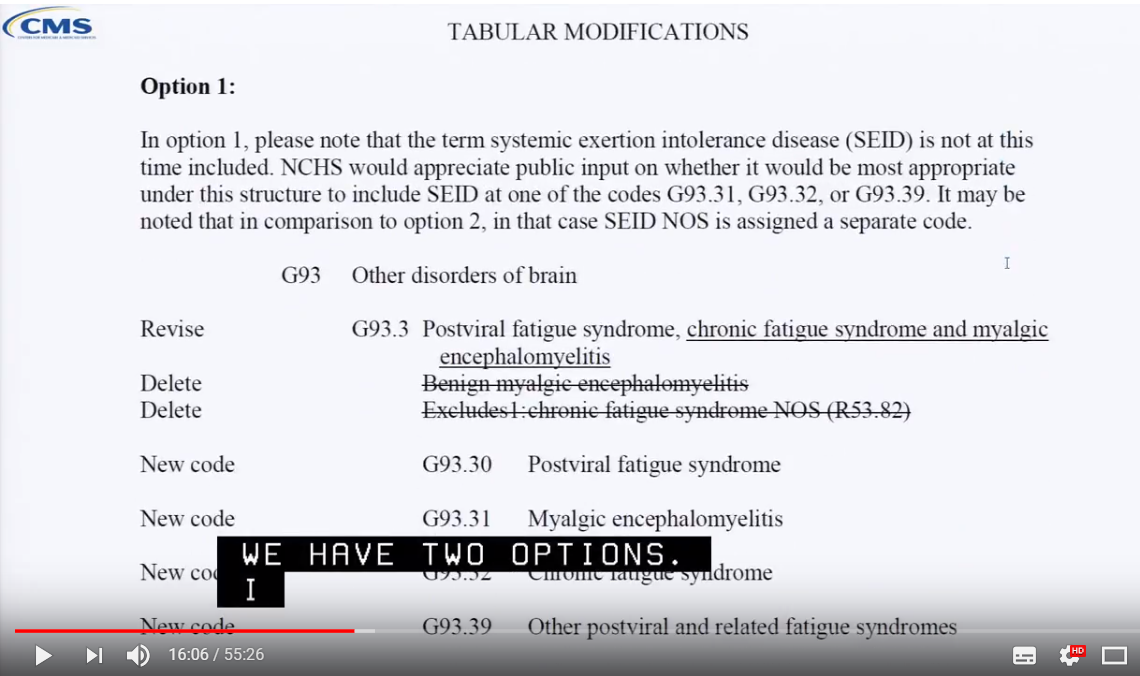
Note that the proposal for changes to the Alphabetical Index includes the proposal to add the term
Systemic exertion intolerance disease [SEID] G93.32
to the
Index, indexed to proposed new sub-code:
G93.32, which is the proposed new sub-code for proposed new ICD-10-CM term:
G93.32 Myalgic encephalomyelitis/chronic fatigue syndrome
with the following Inclusion terms proposed under
G93.32 Myalgic encephalomyelitis/chronic fatigue syndrome:
Chronic fatigue syndrome
ME/CFS
Myalgic encephalomyelitis