Dx Revision Watch
Senior Member (Voting Rights)
ICD-11 Proposal Mechanism:
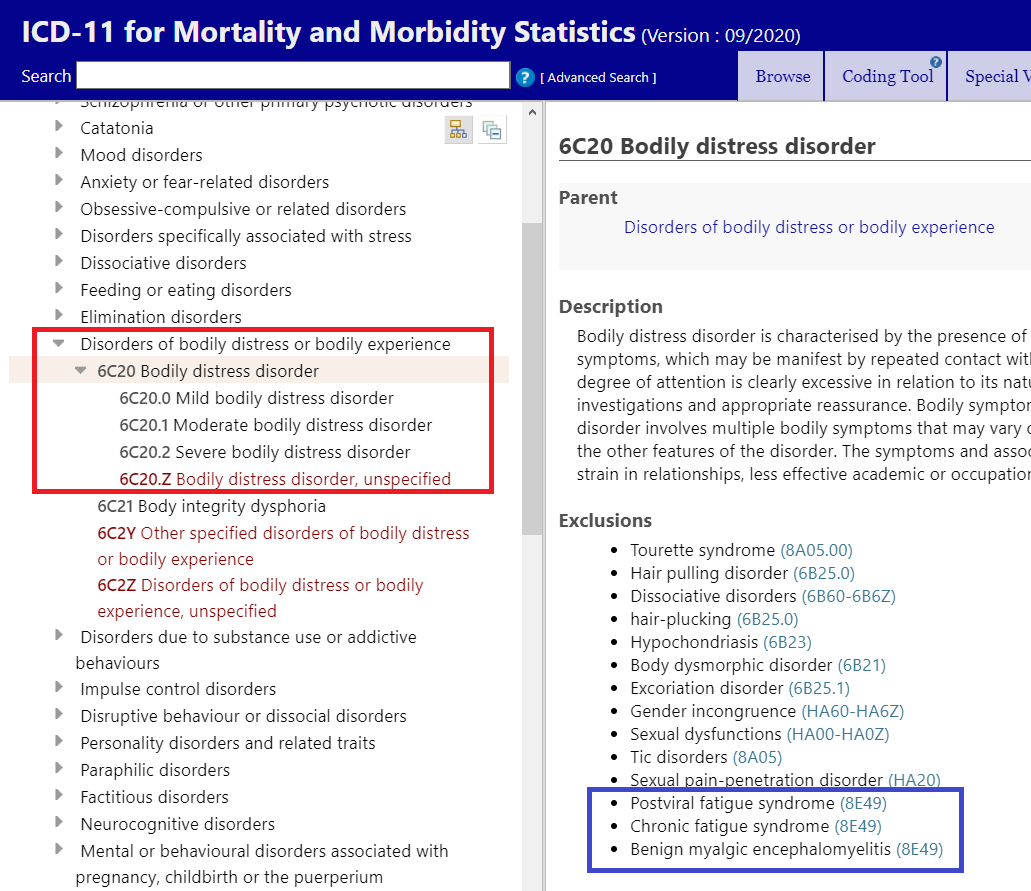
A change of Definition/Description proposal for 6C20 Bodily distress disorder was submitted to the ICD-11 Proposal Mechanism by the WHO's Dr Geoffrey Reed on February 29, 2020:
https://icd.who.int/dev11/proposals...lGroupId=41ee2f01-05cf-4883-82f3-db2a553f5258
Content Enhancement Proposal
Originator: Geoffrey Reed #2A1H
Bodily distress disorder
Current text:
Bodily distress disorder is characterized by the presence of bodily symptoms that are distressing to the individual and excessive attention directed toward the symptoms, which may be manifest by repeated contact with health care providers. If another health condition is causing or contributing to the symptoms, the degree of attention is clearly excessive in relation to its nature and progression. Excessive attention is not alleviated by appropriate clinical examination and investigations and appropriate reassurance. Bodily symptoms are persistent, being present on most days for at least several months. Typically, bodily distress disorder involves multiple bodily symptoms that may vary over time. Occasionally there is a single symptom—usually pain or fatigue—that is associated with the other features of the disorder.
Proposed addition (in brown):
Bodily distress disorder is characterized by the presence of bodily symptoms that are distressing to the individual and excessive attention directed toward the symptoms, which may be manifest by repeated contact with health care providers. If another health condition is causing or contributing to the symptoms, the degree of attention is clearly excessive in relation to its nature and progression. Excessive attention is not alleviated by appropriate clinical examination and investigations and appropriate reassurance. Bodily symptoms are persistent, being present on most days for at least several months. Typically, bodily distress disorder involves multiple bodily symptoms that may vary over time. Occasionally there is a single symptom—usually pain or fatigue—that is associated with the other features of the disorder. The symptoms and associated distress and preoccupation have at least some impact on the individual’s functioning (e.g., strain in relationships, less effective academic or occupational functioning, abandonment of specific leisure activities).
Proposal status: Submitted
Rationale:
These are minor changes to be more consistent with the expanded diagnostic guidance for mental disorders. Name of chapter was corrected. The necessary impact on functioning has been made clearer.
References
There are no references attached for this proposal item
-----------------------------------------------------------
It is unclear what "Name of chapter was corrected." refers to. I have asked for clarification. (I suspect it may have been included due to a pasting error inherited as a result of using part of the Rationale text for other disorders submitted in that batch.)
This proposal for additional text to be added to the BDD Definition/Description text is one of around 40 submissions that were batch submitted on February 29 for various disorders in the Mental, behavioural, and neurodevelopmental disorders chapter.
These include revisions to the texts for:
Hypochondriasis (Substantive changes to the Definition/Description text)
Current text:
Hypochondriasis is characterized by persistent preoccupation with or fear about the possibility of having one or more serious, progressive or life-threatening diseases. The preoccupation is associated with catastrophic misinterpretation of bodily signs or symptoms, including normal or commonplace sensations, and is manifest either in repetitive and excessive health-related behaviours or in maladaptive avoidance behaviours related to health. The preoccupation or fear is not simply a reasonable concern related to a specific context of the patient, and persists or reoccurs despite appropriate medical evaluation and reassurance. The symptoms result in significant distress or significant impairment in personal, family, social, educational, occupational or other important areas of functioning.
Proposed change:
Hypochondriasis is characterized by persistent preoccupation or fear about the possibility of having one or more serious, progressive or life-threatening illnesses. The preoccupation is accompanied by either: 1) repetitive and excessive health-related behaviours such as repeatedly checking of the body for evidence of illness, spending inordinate amounts of time searching for information about the feared illness, repeatedly seeking reassurance (e.g., arranging multiple medical consultations); or 2) maladaptive avoidance behaviour related to health (e.g., avoids medical appointments). The symptoms result in significant distress or significant impairment in personal, family, social, educational, occupational or other important areas of functioning.
Rationale
These are minor changes to be more consistent with the expanded diagnostic guidance for mental disorders. Substantive meaning of description is the same, but language has been clarified.
-----------------------------------------------------------
For the following Dissociative neurological symptom disorder terms, the change is described as: "These are minor changes to be more consistent with the expanded diagnostic guidance for mental disorders. Name of chapter was corrected. The term 'health condition' has been changed to 'medical condition' as this is the term that the TAG decided to use throughout.
"or neurodevelopmental disorder" has also been inserted for some of the following, minor typographical errors corrected and in one disorder, an exclusion revised:
Dissociative neurological symptom disorder
Dissociative neurological symptom disorder, with Parkinsonism
Dissociative neurological symptom disorder, with facial spasm
Dissociative neurological symptom disorder, with dystonia
Dissociative neurological symptom disorder, with tremor
Dissociative neurological symptom disorder, with myoclonus
Dissociative neurological symptom disorder, with chorea
Dissociative neurological symptom disorder, with movement disturbance
Dissociative neurological symptom disorder, with gait disturbance
Dissociative neurological symptom disorder, with paresis or weakness
Dissociative neurological symptom disorder, with speech disturbance
Dissociative neurological symptom disorder, with non-epileptic seizures
Dissociative neurological symptom disorder, with other sensory disturbance
Dissociative neurological symptom disorder, with vertigo or dizziness
Dissociative neurological symptom disorder, with auditory disturbance
Dissociative neurological symptom disorder, with visual disturbance
Dissociative neurological symptom disorder, with cognitive symptoms
-----------------------------------------------------------
As these changes are being submitted by the WHO's lead Managing Editor for the Mental disorder chapter in order to align with the texts in the draft CDDG, I anticipate they will be marked as approved and implemented within the next few days.
------------------------------------------------------------
Edited to add: This batch of 40 proposals for minor changes to align description texts with the draft CDDG are now marked as Implemented.
A change of Definition/Description proposal for 6C20 Bodily distress disorder was submitted to the ICD-11 Proposal Mechanism by the WHO's Dr Geoffrey Reed on February 29, 2020:
https://icd.who.int/dev11/proposals...lGroupId=41ee2f01-05cf-4883-82f3-db2a553f5258
Content Enhancement Proposal
Originator: Geoffrey Reed #2A1H
Bodily distress disorder
Current text:
Bodily distress disorder is characterized by the presence of bodily symptoms that are distressing to the individual and excessive attention directed toward the symptoms, which may be manifest by repeated contact with health care providers. If another health condition is causing or contributing to the symptoms, the degree of attention is clearly excessive in relation to its nature and progression. Excessive attention is not alleviated by appropriate clinical examination and investigations and appropriate reassurance. Bodily symptoms are persistent, being present on most days for at least several months. Typically, bodily distress disorder involves multiple bodily symptoms that may vary over time. Occasionally there is a single symptom—usually pain or fatigue—that is associated with the other features of the disorder.
Proposed addition (in brown):
Bodily distress disorder is characterized by the presence of bodily symptoms that are distressing to the individual and excessive attention directed toward the symptoms, which may be manifest by repeated contact with health care providers. If another health condition is causing or contributing to the symptoms, the degree of attention is clearly excessive in relation to its nature and progression. Excessive attention is not alleviated by appropriate clinical examination and investigations and appropriate reassurance. Bodily symptoms are persistent, being present on most days for at least several months. Typically, bodily distress disorder involves multiple bodily symptoms that may vary over time. Occasionally there is a single symptom—usually pain or fatigue—that is associated with the other features of the disorder. The symptoms and associated distress and preoccupation have at least some impact on the individual’s functioning (e.g., strain in relationships, less effective academic or occupational functioning, abandonment of specific leisure activities).
Proposal status: Submitted
Rationale:
These are minor changes to be more consistent with the expanded diagnostic guidance for mental disorders. Name of chapter was corrected. The necessary impact on functioning has been made clearer.
References
There are no references attached for this proposal item
-----------------------------------------------------------
It is unclear what "Name of chapter was corrected." refers to. I have asked for clarification. (I suspect it may have been included due to a pasting error inherited as a result of using part of the Rationale text for other disorders submitted in that batch.)
Note: The "expanded diagnostic guidance for mental disorders" is a reference to the Clinical Descriptions and Diagnostic Guidelines (CDDG) for ICD‐11 Mental, Behavioural and Neurodevelopmental Disorders (an equivalent publication to ICD-10's "Blue Book").
The CDDG provides expanded clinical descriptions, essential (required) features, boundaries with other disorders and normality, differential diagnoses, additional features, culture-related features and codes for all mental and behavioural disorders commonly encountered in clinical psychiatry. This companion publication is intended for use by mental health professionals and for general clinical, educational and service use. The WHO has said it planned to release the CDDG "as soon as possible" after WHA's adoption of ICD-11. But it remains unclear whether the CDDG has been finalised and when it is planned to be released.
The CDDG provides expanded clinical descriptions, essential (required) features, boundaries with other disorders and normality, differential diagnoses, additional features, culture-related features and codes for all mental and behavioural disorders commonly encountered in clinical psychiatry. This companion publication is intended for use by mental health professionals and for general clinical, educational and service use. The WHO has said it planned to release the CDDG "as soon as possible" after WHA's adoption of ICD-11. But it remains unclear whether the CDDG has been finalised and when it is planned to be released.
This proposal for additional text to be added to the BDD Definition/Description text is one of around 40 submissions that were batch submitted on February 29 for various disorders in the Mental, behavioural, and neurodevelopmental disorders chapter.
These include revisions to the texts for:
Hypochondriasis (Substantive changes to the Definition/Description text)
Current text:
Hypochondriasis is characterized by persistent preoccupation with or fear about the possibility of having one or more serious, progressive or life-threatening diseases. The preoccupation is associated with catastrophic misinterpretation of bodily signs or symptoms, including normal or commonplace sensations, and is manifest either in repetitive and excessive health-related behaviours or in maladaptive avoidance behaviours related to health. The preoccupation or fear is not simply a reasonable concern related to a specific context of the patient, and persists or reoccurs despite appropriate medical evaluation and reassurance. The symptoms result in significant distress or significant impairment in personal, family, social, educational, occupational or other important areas of functioning.
Proposed change:
Hypochondriasis is characterized by persistent preoccupation or fear about the possibility of having one or more serious, progressive or life-threatening illnesses. The preoccupation is accompanied by either: 1) repetitive and excessive health-related behaviours such as repeatedly checking of the body for evidence of illness, spending inordinate amounts of time searching for information about the feared illness, repeatedly seeking reassurance (e.g., arranging multiple medical consultations); or 2) maladaptive avoidance behaviour related to health (e.g., avoids medical appointments). The symptoms result in significant distress or significant impairment in personal, family, social, educational, occupational or other important areas of functioning.
Rationale
These are minor changes to be more consistent with the expanded diagnostic guidance for mental disorders. Substantive meaning of description is the same, but language has been clarified.
-----------------------------------------------------------
For the following Dissociative neurological symptom disorder terms, the change is described as: "These are minor changes to be more consistent with the expanded diagnostic guidance for mental disorders. Name of chapter was corrected. The term 'health condition' has been changed to 'medical condition' as this is the term that the TAG decided to use throughout.
"or neurodevelopmental disorder" has also been inserted for some of the following, minor typographical errors corrected and in one disorder, an exclusion revised:
Dissociative neurological symptom disorder
Dissociative neurological symptom disorder, with Parkinsonism
Dissociative neurological symptom disorder, with facial spasm
Dissociative neurological symptom disorder, with dystonia
Dissociative neurological symptom disorder, with tremor
Dissociative neurological symptom disorder, with myoclonus
Dissociative neurological symptom disorder, with chorea
Dissociative neurological symptom disorder, with movement disturbance
Dissociative neurological symptom disorder, with gait disturbance
Dissociative neurological symptom disorder, with paresis or weakness
Dissociative neurological symptom disorder, with speech disturbance
Dissociative neurological symptom disorder, with non-epileptic seizures
Dissociative neurological symptom disorder, with other sensory disturbance
Dissociative neurological symptom disorder, with vertigo or dizziness
Dissociative neurological symptom disorder, with auditory disturbance
Dissociative neurological symptom disorder, with visual disturbance
Dissociative neurological symptom disorder, with cognitive symptoms
-----------------------------------------------------------
As these changes are being submitted by the WHO's lead Managing Editor for the Mental disorder chapter in order to align with the texts in the draft CDDG, I anticipate they will be marked as approved and implemented within the next few days.
------------------------------------------------------------
Edited to add: This batch of 40 proposals for minor changes to align description texts with the draft CDDG are now marked as Implemented.
Last edited: