If Dr O'Leary considers the issue that millions of patients worldwide
have already been assigned a diagnosis of Chronic fatigue syndrome in the records of the multiple agencies with which they have to deal is "a small point"; and argues that ICD and SNOMED CT classification and coding is a minor inconvenience that would "catch up" in time, I can only conclude that she has limited understanding of how coding underpins the operation of NHS England and at local NHS Trust level to support strategic planning, commissioning, resource allocation, determining care paths, NHS Quality and Outcomes Frameworks etc.
Once again:
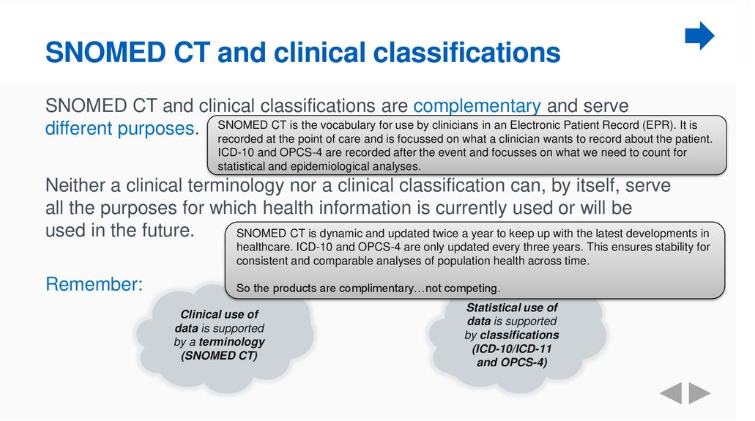
at the point of care, SNOMED CT terminology system is now mandatory for use in primary and secondary care data sets and SNOMED CT Concept codes are mapped to ICD-10 equivalents.
After the encounter, ICD-10 Version: 2016 is mandatory for data compilation.
You cannot have a national health system in which clinicians are being encouraged to apply a long established term (since 1994 in the case of the ICD-10 Index) to a different cohort, when clinicians and coders will be continuing to code that term to
G93.3 and where the term "ME/CFS" contains the
same term that you are proposing should now be applied to a different cohort and will also continue to be coded to G93.3 (and all three terms to 8E49, once ICD-11 is rolled out in the NHS).
I am struggling to see the logic in your proposal.
Every year, NHS Digital publishes the:
NHS Digital National Clinical Coding Standards guidance for coders.
"These national clinical coding standards are for use with the Tenth Revision 5th Edition (ICD-10) when translating diagnoses and other health related problems recorded in a patient’s medical record for morbidity coding.
The classification of diagnoses using ICD-10 is a mandatory national requirement for the NHS Admitted Patient Care (APC) Commissioning Data Set (which includes day cases) and other data sets as outlined in the section below."
The current edition is:
NHS Digital National Clinical Coding Standards ICD-10 5th Edition (April 2020)
PDF:
https://tinyurl.com/y4ogxxu6
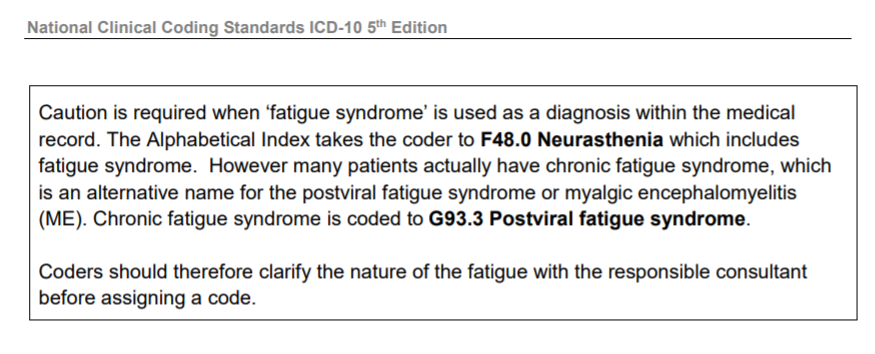
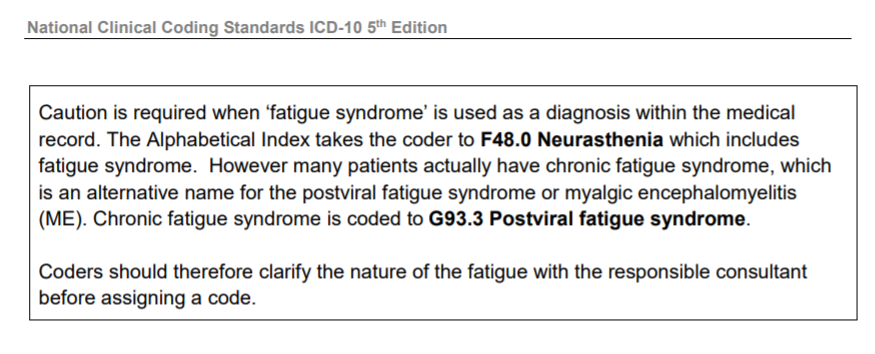
On Page 84:
This note for coders has been included in the NHS Digital Clinical Coding Standards for a number of years.
"Clinical coding
Clinical coding is the translation of medical terminology that describes a patient’s complaint, problem, diagnosis, treatment or other reason for seeking medical attention into codes that can then be easily tabulated, aggregated and sorted for statistical analysis in an efficient and meaningful manner.
(...)
Background
The WHO states that ICD is to permit the systematic recording, analysis, interpretation and comparison of mortality and morbidity data collected in different countries or areas and at different times. The ICD is used to translate diagnoses and other health problems from words into alphanumeric codes, which permits easy storage, retrieval and analysis of data’1.
1 World Health Organisation International Classification of Diseases and Related Health Problems’ ICD-10 Volume 2, 2.1 Purpose and applicability
ICD-10 is a vital component of national data sets, such as Hospital Episodes Statistics (HES) in England, Hospital In-patient Statistics (HIS) in Northern Ireland, Patient Episode Data for Wales (PEDW), Scottish Morbidity Records (SMR), Cancer Registries, National Service Frameworks, Care Pathways, Performance Indicators, Commissioning Data Sets (CDS) and other Central Returns.
The statistical classification underpins key information initiatives that support the monitoring of morbidity and health trends. NHS managers and health care professionals use it locally to support operational/strategic planning and performance management.
For example:
• Statistical uses include study of aetiology (cause or origin) and incidence of diseases, health care planning and casemix.
• Epidemiologists use statistical data to study frequency and occurrence of disease. The aggregation of coded data enables health professionals to identify at risk populations based on demographic, diagnostic or environmental factors.
• Planners and managers use statistical data to review caseloads to: determine specialty needs, inform staffing levels, patient admissions and clinic schedules in hospitals.
• Clinical audit uses coded data to compare patient care and measure outcomes within specialities. Doctors may use extracts of local information for research purposes. The United Kingdom has a mandatory obligation to collect and submit ICD-10 data to the World Health Organisation (WHO) for the production of international statistical and epidemiological data..."
PDF (250 pages):
https://tinyurl.com/y4ogxxu6
-----------------------------------------------------------------
Coding and data analysis is crucial to the operation of the NHS.
SNOMED CT and ICD-10 are embedded into health service electronic record systems. Type a term into the system, like "Chronic fatigue syndrome", and the G93.3 code will be automatically assigned.
And as another poster has said, there are other terms that liaison psychiatry has at its disposal:
ICD-10 Version: 2016
F45.x Somatoform disorder block
F48.0 Fatigue syndrome
R53 Malaise and fatigue
SNOMED CT
SCTID: 887761000000101 Medically unexplained symptoms (finding)
and potentially, Somatic symptom disorder (if approval of IAPT's request is obtained)
and when
ICD-11 MMS has implemented,
MG22 Fatigue (I obtained Exclusions for all three 8E49 terms under MG22.)
6C20 Bodily distress disorder (I obtained Exclusions for all three 8E49 terms under 6C20.)
You cannot kick the issue of ICD-10/SNOMED CT coding, classification and terminology into the long grass just because it doesn't support your proposed paradigm shift.
Nor dodge the question of how you envisage safeguarding the thousands of patients who already have a diagnosis of Chronic fatigue syndrome in their medical records.
To dismiss my concerns around coding as "quibbling" is disturbing and it concerns me enormously how much time and energy members of this forum have had to expend reiterating these points to you.
Yesterday, the WHO Assistant Director-General was flagging up the BMJ Management of Covid-19 Practice Points article on Twitter. I hope not too many clinicians and allied health professionals are going to be reading the Rapid Responses.
Dr O'Leary, you are a US based academic. If you want to set yourself up as an effective advocate for ME and CFS patients, it is essential that you first consult with patients and with patient organisations before putting out statements like:
The term “chronic fatigue syndrome” names a psychiatric condition that sometimes develops in reaction to acute viral infection.[2] [3] [4] It is essentially deconditioning that arises from inactivity when patients embrace faulty illness beliefs.
or:
Criteria for BDD are not particularly problematic for ME patients. They are compatible with construing ME as a biological disease.
and not respond, dismissively, with:
I appreciate all the discussion, though I can't possibly answer all these small points.
when you are challenged on your illogical proposals.