Iniital thoughts
Hats off to Lenny Jason and colleagues for pulling off and a huge and significant study.
This is the first truly prospective study of post-infectious ME/CFS. The importance of prospective studies is that measuring what happens before the illness starts allows researchers to identify causal factors. Most studies in ME/CFS can only find associations with illness, which can’t distinguish cause from effect.
This was a huge study. 4700 students were enrolled between March 2014 and June 2018. Most of them were in their first year and about half of each incoming class enrolled in the study. More than 95% of those who enrolled completed the surveys (nine of them, I think) and gave a blood sample.
The paper says that students were compensated fortaking part, which looks like a smart move, because these participation rates are incredible.
Out of this huge cohort of 4500 students, 238 (5%) developed infectious mononucleosis (glandular fever) by the end of June 2019. 55 of these (23%) met at least one of the criteria for ME/CFS are (CCC, Fukuda and IOM). 20 students meant at least 2 criteria and were classified as severe (
@Andy no further qjustification for this was given).
157 students no longer had symptoms at six months and were classified as recovered.
Key results
Comparing those with mono who recovered with those who developed ME/CFS, there appear to be two important results from this study:
1. There are no siginficant differences between the two groups on the measured psychological factors of stress, coping, anxiety or depression at baseline. That seriously undermines psychosocial theories of the illness. If they need undermining any further.
2. "In a previous study, we identified mononucleosis severity as a risk factor for severe ME/CFS. That relationship was found in the present analysis as well (p = 0.04; data not shown)". and the P value isn't impressive but it also ties in with findings from the Dubbo study. And with Peter White's infectious mono study, which found that days of bedrest predicted CFS. They don't say how severity was measured.
Otherwise, not so much to see, I fear
Based on my first reading of the paper, there is otherwise not a huge amount here. There are some differences but I'm not sure if the authors have corrected sufficiently for the very high number of comparisons(e.g they use results from 12 different scales but use a p value of 0.01). And in any case the differences appear to be quite small even if they are significant.
I'd be very to know if
@Jonathan Edwards thinks cytokine differences given in table 3 are likely to mean very much.
Some issues to discuss
This situation is disappointing. There are a few methodological issues that may or may not be relevant. I would appreciate the views of others.
1. Data and blood samples were taken "within six weeks of diagnosis". That strikes me as quite a wide window and I thought it was much shorter for both Dubbo and the Peter White study. This raises the possibility that, for at least some people, the data and blood sample were collected after the main action was over.
2. I am not convinced that the threshold for "substantial reduction in activities# was especially strong.
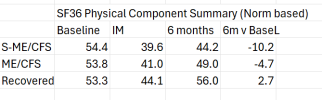
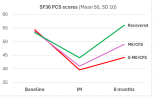
Surprisingly, the study does not use the SF36 Physical Functioning PF scale, which is the scale used by most researchers in diagnosis. Instead, the authors define substantial reduction as "scoring at or below at least two of three cut-offs on the SF 36: role physical <= 50, social functioning l<= 62.5, and vitality <= 35.
Also, this study uses the DePaul symptom questionnaire and its definition of PEM. There are reasons to question whether that actually captures PEM, with the risk that sweeps people into a diagnosis that perhaps shouldn't be there.
However, all diagnosed cases did have a medical exam and physical and psychological assessment.
Certainly, the very high proportion of people with IM developing ME/CFS at six months (23%) is surprisingly.
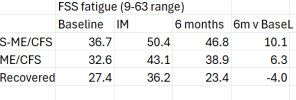
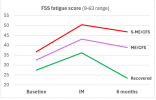
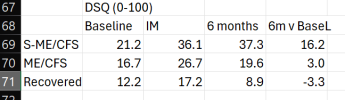
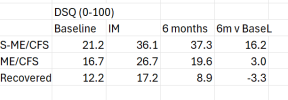
3. For the non-severe ME/CFS cases (i.e. meeting only one criteria, which the paper says was almost always Fukuda) the increases in fatigue and DSQ scores from baseline are modest.
DSQ symptom scores increased from 17 at baseline to 20 at six months, while the fatigue score increased from 33 to 39. The severe ME/CFS scores showed a bigger incremental increase, but it still wasn't huge. Certainly, I think these small incremental increases cast some doubt on the validity of the single-criteria-meeting standard ME/CFS group.
Okay, I am done.
Added: apologies for not quoting people's contributions; not easy on an iphone and trying to avoid triggering the next bloody migraine with too much screen use.