Jonathan Edwards
Senior Member (Voting Rights)
B12 Testing is not the name of an antibody,
I know but the paper you cited, as far as I can see was to do with something called B12 that has nothing to do with the vitamin, just has the same name.
B12 Testing is not the name of an antibody,
We are at the stage of chickens
There is a lot more but is you go way back or list those that treat and talk about Mast cell
As far as Mast Cell and vitamin deficiency there is a lot of work but not joined up and most choric long term conditions such a diabetes, Lupus and MS have associations to vit deficiency and mast cell so starting with the old research

Serum tryptase measured with B12 and G5 antibody-based immunoassays in mastocytosis patients and its relation to histamine turnover - PubMed
Serum tryptase was measured with the B12 and G5 antibody-based immunoassays in 25 adult patients with mastocytosis and in 18 controls. Twelve patients had uncomplicated cutaneous mastocytosis (urticaria pigmentosa) and 13 had urticaria pigmentosa with systemic symptoms. Tryptase levels were...pubmed.ncbi.nlm.nih.gov
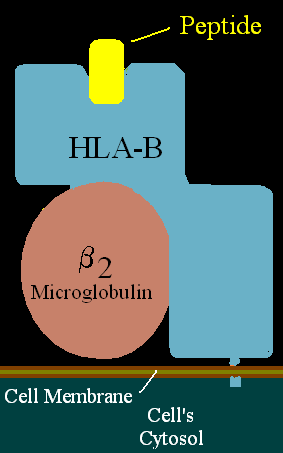
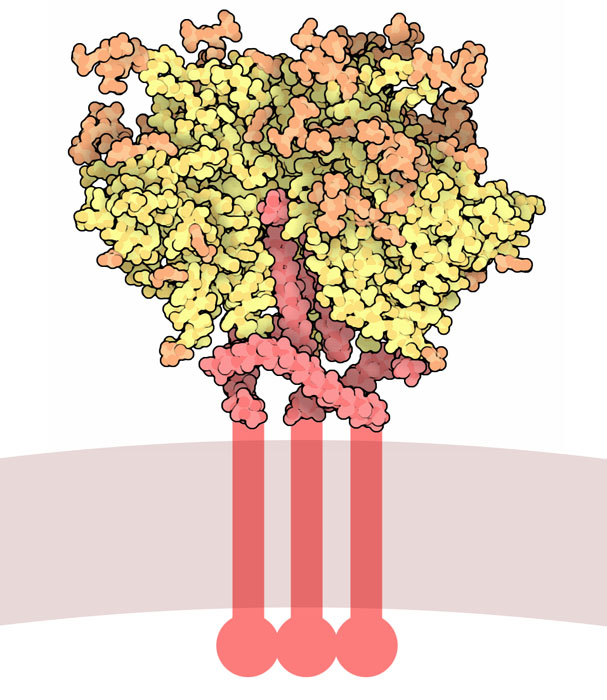
The TT test relies on 2 monoclonal antibodies with different specificities: “B12” for capture and “G4” for detection, the latter in its Fab’2 form, “B12” also able to dissociate tryptase tetramers and maintain their monomeric status.
Some information found trough a web search about the B12 antibody which this article seems to be about:
Lots of people with orthostatic intolerance have below 30 HR increase in tilt tables, so a «normal» response might still be OI.such as lightheadedness from an eating disorder that they insist on explaining away as POTS, despite a normal tilt table
For the UK folks who are concerned about this, I’m curious if gastroparesis is also on your radar. My husband is a physician in the US, and we are becoming very suspicious that there is a large number of questionable gastroparesis diagnoses in the same population that this thread is about.
(It is not that hard to end up with a false positive on a motility test, for those who don’t know.)
My husband is well informed about ME, and most of the patients he sees with the constellation of diagnoses mentioned in this thread definitely do not have it. It seems the primary issue for a lot of them is a GI one. I hesitate to say this because I’m afraid of being misinterpreted, but a good number of them really do have problems that are psychiatric in origin, such as lightheadedness from an eating disorder that they insist on explaining away as POTS, despite a normal tilt table. It’s pretty clear to me that doctors are seeing this type of patient fairly often now and lumping ME patients with these extra diagnoses in with them. In our area of the US, patients getting these diagnoses to explain ME-related symptoms would be a small minority of the people with these diagnoses, and most doctors are totally unaware of them.
[Edited for clarity]
I know, and so does my husband because I’m one of them, actually. There was nothing to actually suggest POTS in this case. She was just stuck on that explanation. It happens.Lots of people with orthostatic intolerance have below 30 HR increase in tilt tables, so a «normal» response might still be OI.
I have no idea about the gastroparesis, but the symptoms seem generic enough to be a candidate for misdiagnosis or wrong self-diagnosis.
Yes, that is really concerning. Totally agree.This is of particular concern, given the problems that those with very severe ME/CFS and feeding problems have already getting appropriate medical management. If there is over diagnosis/misdiagnosis of gastroparesis it is going to make the life of those needing non-oral feeding even more of a nightmare.
Whoops, sorry, I totally missed this somehow. Yes, definitely agree. Lots of things can cause those symptoms. It would be pretty easy for a patient or a doctor to mess that one up.I have no idea about the gastroparesis, but the symptoms seem generic enough to be a candidate for misdiagnosis or wrong self-diagnosis.
I think this is a dangerous position to take. You seem to be suggesting that you (or others) can tell which patients' GI symptoms have a physical basis and which are produced by the mind. I don't think that is a useful distinction but even if it was I have no confidence that doctors can correctly attribute the cause of symptoms in this way. We don't know what process is causing these symptoms, and so suggesting that some should be treated differently because they are placed in a questionable group I don't think is helpful. Trying to attribute symptoms to unknown causes is why ME/CFS has been considered psychiatric in the past (and for many still today).I hesitate to say this because I’m afraid of being misinterpreted, but a good number of them really do have problems that are psychiatric in origin, such as lightheadedness from an eating disorder that they insist on explaining away as POTS, despite a normal tilt table. It’s pretty clear to me that doctors are seeing this type of patient fairly often now and lumping ME patients with these extra diagnoses in with them. In our area of the US, patients getting these diagnoses to explain ME-related symptoms would be a small minority of the people with these diagnoses, and most doctors are totally unaware of them.
Sorry, I think I was unclear. The patients who have GI complaints and the patients who have clear psychiatric problems are not the same patients. My husband explicitly said the medical complaint when someone presents with hEDS/MCAS/POTS is usually GI and probably legitimate, though not likely caused by the claimed diagnosis.You seem to be suggesting that you (or others) can tell which patients' GI symptoms have a physical basis and which are produced by the mind.
I find it rather amusing that there is this assumption by some that ME/CFS patients want to claim they have something called MCAS.
