Andy
Senior Member (Voting rights)
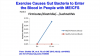
Open access at https://www.mdpi.com/2075-4418/9/3/70Post-exertional malaise (PEM) is a cardinal predictive symptom in the definition of Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS). If the cases overexert themselves they have what is termed “payback” resulting in a worsening of symptoms or relapse which can last for days, weeks or even months. The aim was to assess the changes in biochemistry associated with the cases self-reported PEM scores over a 7-day period and the frequency of reporting over a 12-month period.
Forty-seven ME/CFS cases and age/sex-matched controls had a clinical examination, completed questionnaires; were subjected to standard serum biochemistry; had their serum and urine metabolomes analyzed in an observational study. Thirty-five of the 46 ME/CFS cases reported PEM in the last 7-days and these were allocated to the PEM group. The principal biochemical change related to the 7-day severity of PEM was the fall in the purine metabolite, hypoxanthine. This decrease correlated with alterations in the glucose:lactate ratio highly suggestive of a glycolytic anomaly. Increased excretion of urine metabolites within the 7-day response period indicated a hypermetabolic event was occurring. Increases in urine excretion of methylhistidine (muscle protein degradation), mannitol (intestinal barrier deregulation) and acetate were noted with the hypermetabolic event.
These data indicate hypoacetylation was occurring, which may also be related to deregulation of multiple cytoplasmic enzymes and DNA histone regulation. These findings suggest the primary events associated with PEM were due to hypoacetylation and metabolite loss during the acute PEM response.