The consistent finding is reduced workload (usually measured in watts) at the first ventilatory threshold (VT1, sometimes known as the gas exchange threshold (GET)) between day 1 and day 2.
It is not influenced by voluntary factors as the workrate is fixed - the participant must put out the same amount of power at the same rate of increase, else the test is aborted.
All of this begs the question, what is the gas exchange threshold/why does it occur?
I'd first like to start by saying what it is not.
The VT1/GET is not a point at which the participant will suddenly feel out of breath. There is a second ventilatory threshold, known as the respiratory compensation point which occurs at around 90% of VO2Max where participants (including healthy athletes) start to hyperventilate to compensate for reduced blood PH. At this point, some participants may report feeling out of breath, but not all do. (also, COPD patients may report feeling out of breath at much lower levels of exertion)
The VT1/GET is not a point at which the muscles suddenly run out of oxidative/mitochondrial capacity, indeed it happens well below VO2Max.
The VT1/GET is not synonymous with an 'anerobic threshold', nor is it the same as a 'lactate threshold' which the point at which lactate accumulates significantly in the blood (and thus is additionally related to things like the kinetics of lactate transport).
The VT1/GET is an artefact of the ramped exercise protocol itself. Under uncontrolled exercise conditions, or controlled conditions where there is not a constant increase in workrate (examples include CPETs while fin-swimming), there may not be a clear transition point and the VT (or an anerobic threshold) is not a consequence of reaching a particular heart rate.
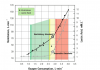
The VT1/GET is a non linearity of the graph when VO2 (Volume of O2 consumed) is plotted against VCO2 (Volume of CO2 exhaled). The VT1 can also be indicated using the ventilatory equivalent method, plotting VE/VO2 and VE/VCO2 on the same graph and noting the point where VE/VO2 increases significantly, while VE/VCO2 remains flat (where VE is minute ventilation).
The reason for this non-linearity has often been debated in an chicken or egg type manner. Is it primarily due to a non-linear increase in motor drive, or a shift in nonlinear shift in metabolic balance versus force output? I suggest both are necessary, since they inevitably lead to the other, causing the clear nonlinearity in the graph.
There is a transition in metabolic balance (from aerobic to non-aerobic metabolism) as higher threshold motor units are recruited, which have a lower balance of oxygen consumption versus force output due to physiological reasons (lower muscle fibre capillarisation, increased O2 diffusion distance etc.)
An aside, the ventilatory drive itself is ramped up in parallel with the increase motor drive (upstream of the motor cortex). Also note that autonomic responses (heart rate and blood pressure) lag behind and react to the change in ventilation. Additionally, note that there isn't a clear pattern of O2 Pulse (VO2/Heart rate) differences at VT1, suggesting that the observed differential between the two days likely isn't due to altered autonomic drive of the heart.
So why is there a reduction in workrate at VT1 between the two days in most ME/CFS patients (in 10+ studies), but not controls?
There are several possible answers:
-due to peripheral motor units being fatigued earlier (such as less optimal firing rates, less force output for a given motor drive) due to metabolic factors
-significantly altered muscle capillary blood flow leading to altered O2 kinetics
-due to stimulation of
Group III/IV muscle afferents, which alters the balance between ventilatory drive and motor cortex excitability.
-the brain decided to completely re-wire it's afferent signals and bypass all of the normal feedback mechanisms that prevent this from happening for shits and giggles. (Note, the signalling of the fatigue related muscle afferents is much more complex than most other forms of pain and cannot be explained by typical pain central sensitisation models or experiments (in experiments, the phenomena is almost always transient, rather than chronic) as there are more systems involved - the proprioceptive system, the motor drive system (various supplementary areas), and the fatigue-related pain system - all of which have to fail, given the feedback between these systems that prevents things from going out of wack)