I use the following:
Heart rate monitor:
- for resting HR: The standard recommendation is to take RHR first thing in the morning but that doesn't work for me; my HR upon waking is extremely erratic and random and probably most linked to how recently I turned over in bed. So I take RHR mid-morning and this tracks my current state of health relatively well but it has no predictive value.
- for peak HR: I have POTS that worsens with PEM. If I cannot keep my HR below 125 during my morning routine I know I'm heading for either PEM or a coldsore reactivation (always comes with significant flu-like symptoms these days).
- for pacing: trying to stay below my anaerobic threshold is difficult with POTS but even just aiming to stay below it results in fewer episodes of physical exertion induced PEM. I used to use an audible threshold alarm, and sometimes still do now, to learn about the HR impact of a new kind of activity but mostly I keep the alarm off now because with POTS it gets triggered so often it becomes maddening. I'm pretty good now at remembering to glance at the monitor regularly.
- for HRV: my heart rate monitor does a kind of heart rate variability based “fitness” test. This tracks my current state of health very well. An unexpectedly low reading is also a warning sign I'm about to hit PEM or a viral flare. Sadly this indicator comes too late to stop the damage but at least it gives me a few hours notice to cancel any plans.
My HR monitor also measures steps and sleep duration and quality but the data is meaningless in my case. The step count seems erratic and doesn't relate well to my actual level of activity nor to whether PEM results or not. The sleep measurements are plain nonsense. I don't know if that's because I always end up sleeping with my HR monitor bearing wrist jammed under my body resulting in faulty readings or whether my sleep quality is so abnormal that a monitor calibrated for healthy people doesn't work.
In summary, the HR monitor data correlates well with symptom severity. Changes in HR are also the earliest sign I have found yet of PEM and viral flares, i.e. changes in HR precede other symptoms by a few hours. Unfortunately starting aggressive resting as soon as HR changes register does not stop the PEM or viral flare.
Using HR monitoring to prevent PEM by staying below my anaerobic threshold as much as possible is only partially effective but makes enough of a difference to definitely be worth doing.
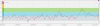
An indirect positive effect of HR monitoring is that it objectively confirms physiological changes when I'm feeling more symptomatic. This serves as a good psychological fortification when confronted with yet another “it's all in your head” argument. I find some people who don't accept verbal explanations can be convinced by some nice heart rate graphics. Like the two below. Both taken over 25 minutes of complete rest, flat on my back doing absolutely nothing, at the same time of day. One the day before a doctor's visit, the other the day after the visit. No prizes for guessing which is which.

 Blood pressure monitor:
Blood pressure monitor:
I got one of these pre-diagnosis when dizziness was one of my major symptoms and I wanted to figure out if BP had anything to do with it (it did). These days I only check sporadically because I eat industrial quantities of salt for my POTS and want an early warning sign of increasing BP (so far all good).
Blood glucose & ketone monitor:
This wasn't planned monitoring, I “inherited” the monitor so thought I might as well have a play with it.
It showed, to my surprise, that while my glucose readings are ok when I'm at my ME baseline, during PEM they swing all over the place, both too high and too low. Additionally, the worse my ME the more likely I'm in ketosis (despite not actually eating keto).
All this is of little practical use to me and I haven't continued regular monitoring (cost of test strips, dislike of finger pricking) but I wonder if this could be a useful research angle, glucose dysregulation in PEM?
Wish list:
Would quite like to do some thorough cortisol and other hormone testing, variations throughout a good day versus a bad day, and repeated regularly, that sort of thing. I think that could give some useful information but it's not a realistic option for now. The same would apply for microbiome & virome tracking.
