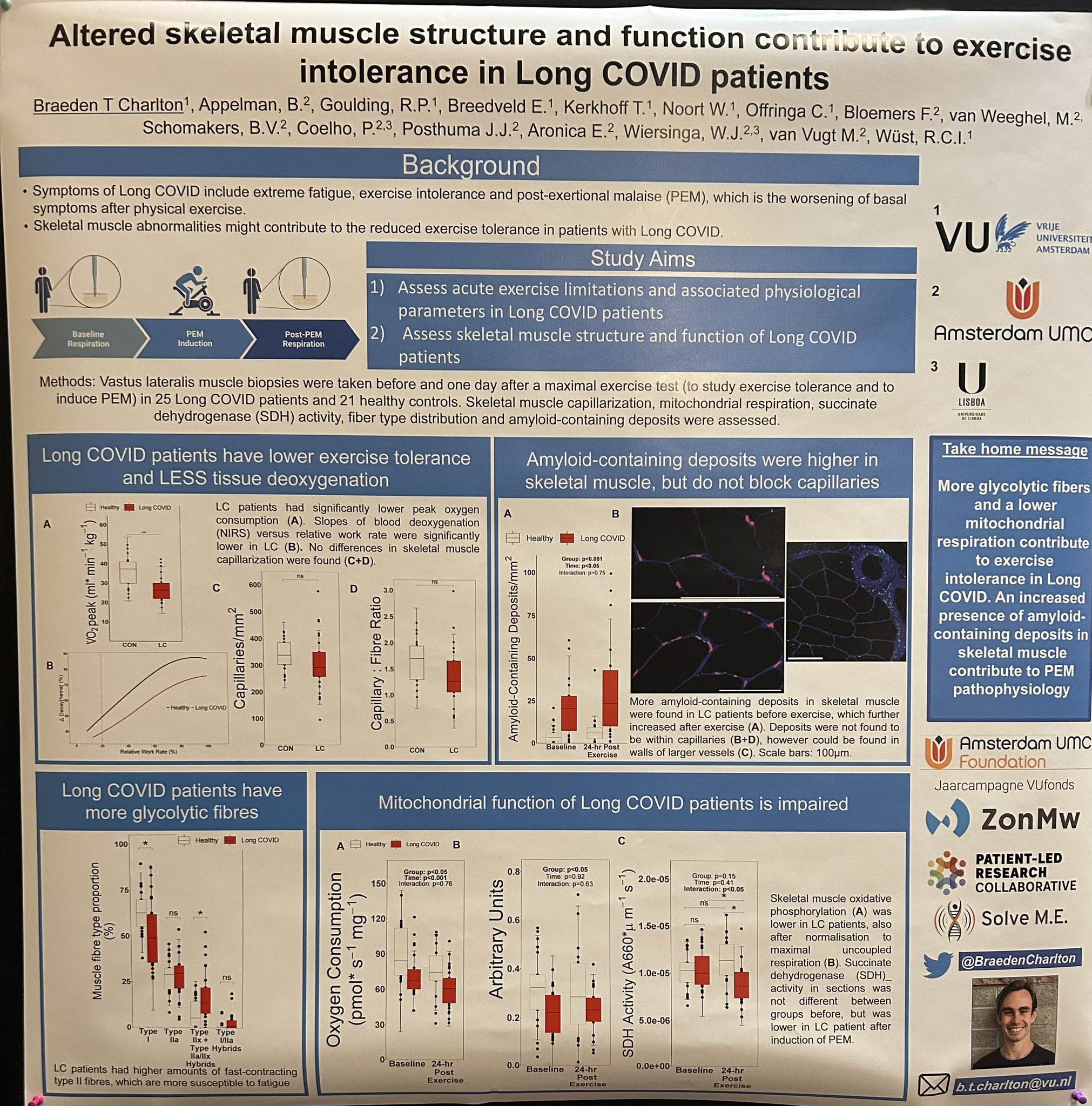
Looks interesting, will be good to follow what Wuest and his team do. I don't know much about how to interpret muscle histological data like this, but - like with the WASF3 paper - I'm concerned about what the effect of deconditioning will have on muscles and therefore these results. Would be good to have disease controls who are deconditioned as a part of their illness. Maybe major depressive disorder you might expect to be less mobile? Or paralysis? Not sure.
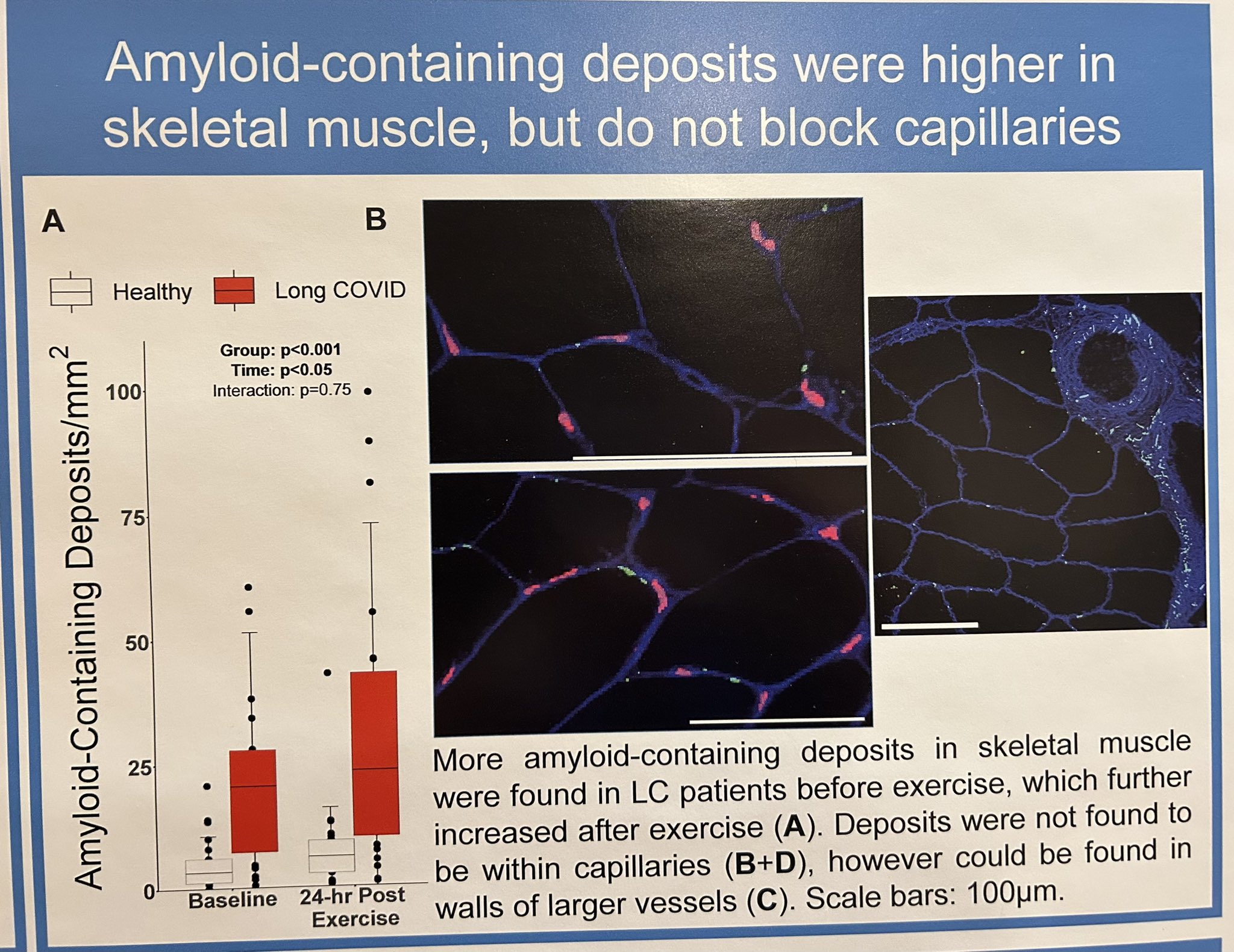
Looks like the PEM associated differences are of amyloid deposition, and of 'necrosis' pictured here from the first poster:
View attachment 20269
Again I don't know what I'm looking at in that histology figure, is there someone who knows more who's able to comment? Is necrosis a normal part of muscle damage after exercise? maybe
@Snow Leopard knows? I think I've seen them comment on this kind of thing before.
They say oxygen consumption rate is lower in muscle from long covid patients, which would be consistent with what Hwang et al say in their WASF3 paper (although for ME not long covid). Looks like they're arguing (in the second poster) that long covid patients have more glycolytic fibres, so maybe that links up with the reduction in citric acid cycle metabolites seen in the first poster (if these cells have reduced oxidative phosphorylation). We can't see their methods obviously so can't scrutinise that yet.