https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3028106/
Chronic fatigue syndrome and complement activation
Robert Dennis Geller; Patricia C Giclas
Abstract
Chronic fatigue syndrome and complement activation
Robert Dennis Geller; Patricia C Giclas
Abstract
This report describes a case of chronic fatigue syndrome (CFS) that followed a well-documented episode of acute Epstein–Barr virus (EBV) mononucleosis. All aetiological tests for chronic fatigue were found to be negative or normal, as were immunological tests.
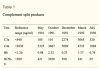
After 2 years of chronic fatigue following the acute illness, measurements of complement split products were performed to test for complement activation. These were positive and remained positive for 14 months, after which the patient then recovered from CFS.