Link to publication here
******************************
Beneficial effects of intermittent intravenous saline infusion in dysautonomic patients with Myalgic Encephalomyelitis/Chronic Fatigue Syndrome: a caseseries
Per Sjogren, Helena Huhmar, Bo Christer Bertilson, Björn A Bragée, Olli Polo
[Line breaks added]
Purpose
Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS) is a debilitating condition with no single, uniformly effective pharmacologic therapy. Dysautonomic features like orthostatic intolerance and postural tachycardia syndrome are common features in ME/CFS, severely affecting the patient´s quality-of-life. Intermittent saline infusion may reduce symptoms associated with dysautonomia, but this has not been tested scientifically in patients with ME/CFS.
In this case-series, 22 patients with ME/CFS and signs of dysautonomia and/or hypovolemia were treated every third week over 9 weeks with intravenous saline (9 mg/mL NaCl), using standard aseptic technique. Symptoms were monitored throughout the treatment regime, and a follow-up evaluation was conducted.
Results
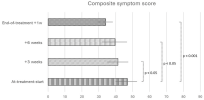
At treatment start, patients were predominantly female (95%), at mean age 46 ± 10 years, and with a mean body hydration percentage of 48 ± 6. Self-reported health status revealed an overall symptom score of 47 ± 13 on a 0-96 scale, a median POTS score of 64 (IQR 16) on a 0-120 scale, and poor measures of quality-of-life (median 25 IQR 25, on a 0-100 scale) and abilityto-work (median 0, IQR 26, on a 0-100 scale).
Following 9 weeks of intermittent saline infusion (mean volume 1600 ± 360 mL), self-reported composite symptom score, quality-of-life and POTS-related symptoms improved significantly (all p<0.001), as did ability-to-work (p<0.05).
Our data derived from a non-controlled case-series indicate health benefits from volume loading with intermittent infusion of saline among patients with ME/CFS, which may stimulate further studies on various forms of intravenous volume loading to patients with ME/CFS and dysautonomia.
Link (Frontiers in Neurology) [Abstract only ahead of publication]
******************************
Beneficial effects of intermittent intravenous saline infusion in dysautonomic patients with Myalgic Encephalomyelitis/Chronic Fatigue Syndrome: a caseseries
Per Sjogren, Helena Huhmar, Bo Christer Bertilson, Björn A Bragée, Olli Polo
[Line breaks added]
Purpose
Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS) is a debilitating condition with no single, uniformly effective pharmacologic therapy. Dysautonomic features like orthostatic intolerance and postural tachycardia syndrome are common features in ME/CFS, severely affecting the patient´s quality-of-life. Intermittent saline infusion may reduce symptoms associated with dysautonomia, but this has not been tested scientifically in patients with ME/CFS.
In this case-series, 22 patients with ME/CFS and signs of dysautonomia and/or hypovolemia were treated every third week over 9 weeks with intravenous saline (9 mg/mL NaCl), using standard aseptic technique. Symptoms were monitored throughout the treatment regime, and a follow-up evaluation was conducted.
Results
At treatment start, patients were predominantly female (95%), at mean age 46 ± 10 years, and with a mean body hydration percentage of 48 ± 6. Self-reported health status revealed an overall symptom score of 47 ± 13 on a 0-96 scale, a median POTS score of 64 (IQR 16) on a 0-120 scale, and poor measures of quality-of-life (median 25 IQR 25, on a 0-100 scale) and abilityto-work (median 0, IQR 26, on a 0-100 scale).
Following 9 weeks of intermittent saline infusion (mean volume 1600 ± 360 mL), self-reported composite symptom score, quality-of-life and POTS-related symptoms improved significantly (all p<0.001), as did ability-to-work (p<0.05).
Our data derived from a non-controlled case-series indicate health benefits from volume loading with intermittent infusion of saline among patients with ME/CFS, which may stimulate further studies on various forms of intravenous volume loading to patients with ME/CFS and dysautonomia.
Link (Frontiers in Neurology) [Abstract only ahead of publication]
Last edited by a moderator: