I don't know if this thread has just slowed down or if others are working on a letter behind the scenes. I think a lot of valid points were raised that prove that Walitt et al.'s interpretation of the EEfRT data is seriously flawed.
I have written a first draft for a letter to be sent to the authors, asking for a correction. Pretty much all arguments have already been made by others on this thread so I take no credit for them - just want to help to string them toghether.
EDIT: I unfortunately will not be able to sign or co-sign a letter as (due to personal circumstances) I prefer to remain anonymous at the moment.
I thus have no concrete plan to send the letter. I hope that others who have more statistical knowledge and academic qualifications than me will take this further.
Incorrect interpretation of ME/CFS patients’ effort preference
In a comprehensive study of patients with post-infectious myalgic encephalomyelitis/chronic fatigue syndrome (PI-ME/CFS), Walitt et al. claim that “
an alteration of effort preference, rather than physical or central fatigue” is a defining feature of the illness.1 Effort preference was defined as
“how much effort a person subjectively wants to exert” and measured using the Effort-Expenditure for Rewards Task (EEfRT). The interpretation of EEfRT results by Walitt and colleagues, however, is highly problematic as it fails to consider that tasks required more effort from patients than from healthy controls.
The EEfRT is a multi-trial experiment that has been used to measure reward motivation in patients with anhedonia, schizophrenia, and other mental disorders. In Walitt et al.’s study of 15 PI-ME/CFS and 17 healthy the EEfRT lasted 15 minutes. In each of the successive trials, participants were instructed to choose between an easy and hard task. Both required several button presses within a limited time frame for successful completion: 30 button presses in 7 seconds for the easy task and 98 button presses in 21 seconds for the hard task. If participants completed the hard task successfully, they had a chance of receiving a higher reward than for completing the easy task. The reward values and probability of receiving it varied across trials and this information was provided to participants before they made their choice. Effort preference was estimated by the proportion of hard task choices. Walitt et al. report that given equal levels and probabilities of reward, healthy controls chose more hard tasks than PI-ME/CFS patients (Odds Ratio, OR = 1.65 [1.03, 2.65], p = 0.04).
The EEfRT requires however that participants can complete the tasks successfully and that the effort needed is equivalent in patients and controls. Treadway et al., the research team that developed the EEfRT and whose protocol was implemented by Walitt et al. with minor modifications, cautioned:
“An important requirement for the EEfRT is that it measure individual differences in motivation for rewards, rather than individual differences in ability or fatigue. The task was specifically designed to require a meaningful difference in effort between hard and easy-task choices while still being simple enough to ensure that all subjects were capable of completing either task, and that subjects would not reach a point of exhaustion.” 2
Several techniques have been introduced in the EEfRT literature to ensure that the test measures reward motivation rather than differences in effort or ability. These include individually calibrating the required number of button presses3, controlling for participants’ motoric ability4, and evaluating whether participants had an adequate completion rate.2
Although Walitt et al. implemented four test trials before the EEfRT started, they did not implement measures to ensure that the effort required to complete tasks was similar in patients and controls. Consequently, PI-ME/CFS patients could only complete 67% of the hard tasks successfully compared to 98% in controls. This was a much larger difference (OR = 27.23 [6.33, 117.14], p < 0.0001) than the group difference in choosing hard over easy tasks. This problem was already evident in the four test trials during which PI-ME/CFS patients could only complete 42% of the hard tasks compared to 82% for controls.
When we added successful completion rate to the statistical model, the difference in hard task choices was no longer significant (OR = 1.19 [0.79, 1.81]).
Walitt et al. did note that during the EEfRT there was no difference in the decline in button-press rate over time for either group for hard tasks. This might indicate that task-related fatigue did not influence the results. There was however a decline in button-press-rate in PI-ME/CFS patients for easy tasks that was not seen in controls. In addition, these measurements only reflect fatigue induced by the 15-minute button-pressing test, not the symptoms and debility participants already had at the start of the EEfRT.
PI-ME/CFS patients were severely disabled with a mean SF-36 physical function score of 31.8 compared to a score of 97.9 for the control group. Reduced psychomotor function5 and impairments in fingertip dexterity and gross movement of the hand, fingers, and arm6 have been reported in ME/CFS patients. Walitt et al. also found that patients in their cohort were unable to maintain force during a hand grip task.1 It is therefore likely that the EEfRT required more effort from PI-ME/CFS patients than from controls. Walitt et al. also reported a strong correlation (R=0.57) between PI-ME/CFS patients’ hard task choices and the ability to maintain force during the grip test. This supports our conclusion that patients’ EEfRT choices reflected motor ability as well as effort preference. No such correlation was found in healthy controls (R=-0.04).
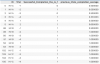
The fact that the group difference in hard task choices was relatively small compared to the larger difference in completion rate, suggests that patients kept trying to succeed on hard tasks, despite past failures. Figure 1 shows the recorded button presses and completion rate per trial for all 31 participants. Several PI-ME/CFS patients had repeated failed attempts to complete the hard tasks (seen as repeated high red bars on the graph), a pattern that was not seen in controls. These findings are contrary to Walitt et al.’s hypothesis that ME/CFS patients prefer to exert themselves less than healthy controls.
View attachment 21419
Figure 1. Button presses per participant for each of the trials they managed to complete during the 15-minute EEfRT. Successful completions are pictured in green while failed attempts are indicated in red.
In conclusion, the EEfRT data indicates that the button-pressing tasks were more difficult for PI-ME/CFS patients than for controls, not that the former have abnormal effort preferences. In the past, ME/CFS patients have repeatedly been ‘victim blamed’ when behavioral consequences of their illness were incorrectly proposed as the cause of their symptoms.7 Considering the negative impact such misattributions may have, we kindly ask Walitt et al to correct their erroneous account of the EEfRT results.
References
1. Walitt, B. et al. Deep phenotyping of post-infectious myalgic encephalomyelitis/chronic fatigue syndrome. Nat Commun 15, 907 (2024).
2. Treadway, M. T., Buckholtz, J. W., Schwartzman, A. N., Lambert, W. E. & Zald, D. H. Worth the ‘EEfRT’? The Effort Expenditure for Rewards Task as an Objective Measure of Motivation and Anhedonia. PLOS ONE 4, e6598 (2009).
3. Fervaha, G. et al. Incentive motivation deficits in schizophrenia reflect effort computation impairments during cost-benefit decision-making. J Psychiatr Res 47, 1590–1596 (2013).
4. Ohmann, H. A., Kuper, N. & Wacker, J. A low dosage of the dopamine D2-receptor antagonist sulpiride affects effort allocation for reward regardless of trait extraversion. Personal Neurosci 3, e7 (2020).
5. Schrijvers, D. et al. Psychomotor functioning in chronic fatigue syndrome and major depressive disorder: a comparative study. J Affect Disord 115, 46–53 (2009).
6. Sanal-Hayes, N. E. M., Hayes, L. D., Mclaughlin, M., Berry, E. C. J. & Sculthorpe, N. F. People with Long Covid and ME/CFS Exhibit Similarly Impaired Dexterity and Bimanual Coordination: A Case-Case-Control Study. Am J Med S0002-9343(24)00091–3 (2024) doi:10.1016/j.amjmed.2024.02.003.
7. Thoma, M. et al. Why the Psychosomatic View on Myalgic Encephalomyelitis/Chronic Fatigue Syndrome Is Inconsistent with Current Evidence and Harmful to Patients. Medicina 60, 83 (2024).