World Psychiatry: Letter to the Editor: Free access, 6 May 2019
Public stakeholders’ comments on ICD‐11 chapters related to mental and sexual health
Johannes Fuss, Kyle Lemay, Dan J. Stein, Peer Briken, Robert Jakob, Geoffrey M. Reed, Cary S. Kogan
Html:
https://onlinelibrary.wiley.com/doi/full/10.1002/wps.20635
PDF:
https://onlinelibrary.wiley.com/doi/epdf/10.1002/wps.20635
...Between January 1, 2012 and December 31, 2017, 402 comments and 162 proposals were submitted on mental, behavioural and neurodevelopmental disorders, sleep‐wake disorders, and conditions related to sexual health. The largest number of submissions related to mental, behavioural and neurodevelopmental disorders focused on compulsive sexual behaviour disorder (N=47), complex post‐traumatic stress disorder (N=26), bodily distress disorder (N=23), autism spectrum disorder (N=17), and gaming disorder (N=11).
(...)
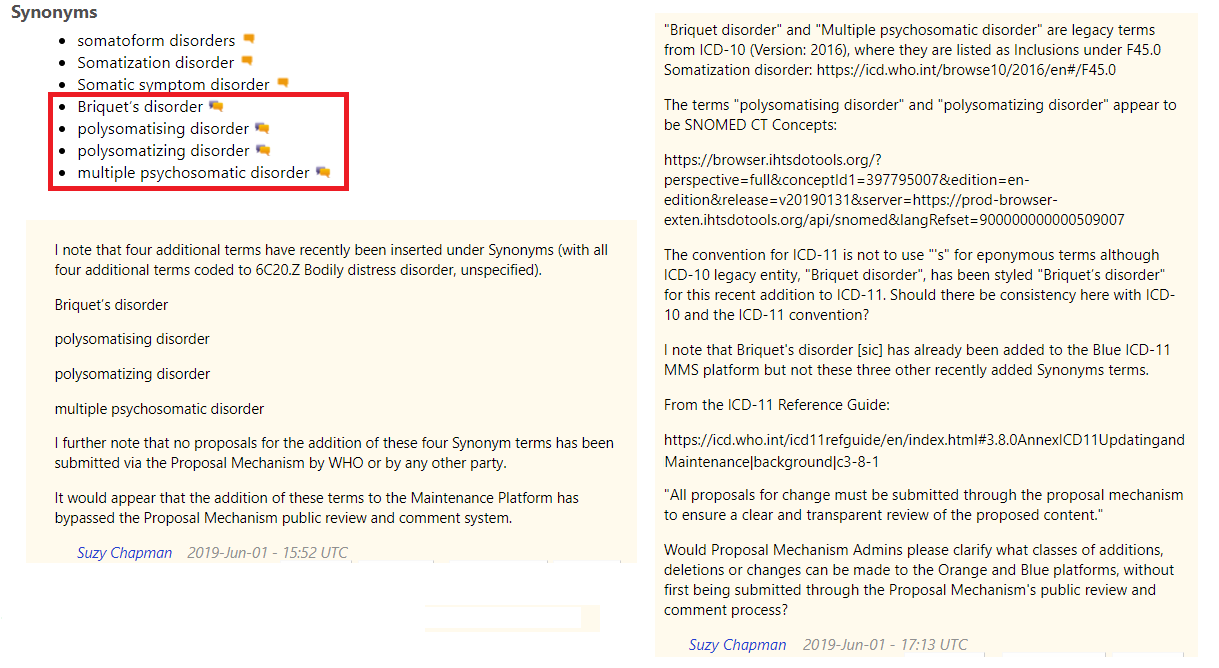
...A majority of submissions regarding bodily distress disorder were critical, but were often made by the same individuals (N=8). Criticism mainly focused on conceptualization (48%; κ=0.64) and the disorder name (43%; κ=0.91). Use of a diagnostic term that is closely associated with the differently conceptualized bodily distress syndrome
5 was seen as problematic.* One criticism was that the definition relies too heavily on the subjective clinical decision that patients’ attention directed towards bodily symptoms is “excessive”. A number of comments (17%; κ=0.62) expressed concern that this would lead to patients being classified as mentally disordered and preclude them from receiving appropriate biologically‐oriented care. Some contributors submitted proposals for changes to the definition (30%; κ=0.89). Others opposed inclusion of the disorder altogether (26%; κ=0.88), while no submission (κ=1) expressed support for inclusion. The WHO decided to retain bodily distress disorder as a diagnostic category
6 and addressed concerns by requiring in the CDDG the presence of additional features, such as significant functional impairment.
----------------------------
*Although WHO's Dr Geoffrey Reed (a co-author of this
Letter to the Editor) had twice agreed with me that there
was potential for confusion between the ICD-11 disorder term, "BDD" and Fink et al (2010) "BDS" and that he would be discussing the issue of BDD terminology with the S3DWG working group (in 2015), ICD Revision did not at any point respond to the specific issue of nomenclature or provide a rationale for not considering an alternative term, which had been raised with them, several times, via Proposal Mechanism Comments and in Submissions.
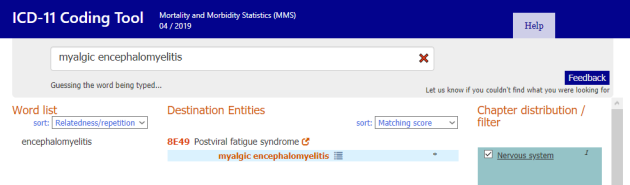
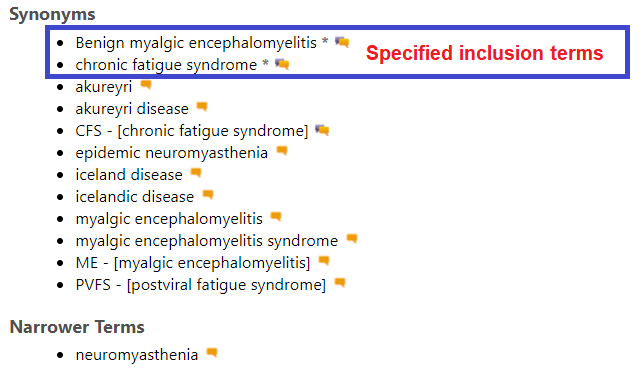
ICD-11's Bodily distress disorder (BDD) has strong conceptual and characterization alignment with DSM-5's Somatic symptom disorder (SSD). Somatic symptom disorder is listed under Synonyms under ICD-11's Bodily distress disorder.
Creed, Henningsen and Fink acknowledge that the Fink et al (2010) BDS construct is differently conceptualized to DSM-5’s SSD; that BDS and SSD have very different criteria and that they capture, or potentially capture, different patient populations [1].
Budtz-Lilly, Fink et al outline some of the conceptual differences between SSD and BDS:
"The newly introduced DSM-5 diagnosis, somatic symptom disorder (SSD), has replaced most of the DSM-IV somatoform disorder subcategories [10]. The diagnosis requires the presence of one or more bothering somatic symptoms of any aetiology and is not based on exclusion of any medical condition (…) BDS and SSD represent two very conceptually different diagnoses. BDS is based on symptom pattern recognition only, and symptoms are thought to be caused by hyperactivity in the central nervous system, whereas SSD criteria are based on prominent positive psycho-behavioural symptoms or characteristics, but no hypothesis of aetiology. BDS is assessed without asking patients about psychological symptoms." [2].
1 Medically Unexplained Symptoms, Somatisation and Bodily Distress: Developing Better Clinical Services, Francis Creed, Peter Henningsen, Per Fink (Eds), Cambridge University Press, 2011.
2 Anna Budtz-Lilly, Per Fink, Eva Ornbol, Mogens Vestergaard, Grete Moth, Kaj Sparle Christensen, Marianne Rosendal. A new questionnaire to identify bodily distress in primary care: The ‘BDS checklist’. J Psychosom Res. June 2015 Volume 78, Issue 6, Pages 536–545.