Andy
Senior Member (Voting rights)
Paywalled at https://www.nature.com/articles/s41385-018-0072-xAbstract
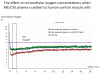
Human mucosal-associated invariant T (MAIT) cell receptors (TCRs) recognize bacterial riboflavin pathway metabolites through the MHC class 1-related molecule MR1. However, it is unclear whether MAIT cells discriminate between many species of the human microbiota. To address this, we developed an in vitro functional assay through human T cells engineered for MAIT-TCRs (eMAIT-TCRs) stimulated by MR1-expressing antigen-presenting cells (APCs). We then screened 47 microbiota-associated bacterial species from different phyla for their eMAIT-TCR stimulatory capacities. Only bacterial species that encoded the riboflavin pathway were stimulatory for MAIT-TCRs. Most species that were high stimulators belonged to Bacteroidetes and Proteobacteria phyla, whereas low/non-stimulator species were primarily Actinobacteria or Firmicutes. Activation of MAIT cells by high- vs low-stimulating bacteria also correlated with the level of riboflavin they secreted or after bacterial infection of macrophages.
Remarkably, we found that human T-cell subsets can also present riboflavin metabolites to MAIT cells in a MR1-restricted fashion. This T–T cell-mediated signaling also induced IFNγ, TNF and granzyme B from MAIT cells, albeit at lower level than professional APC. These findings suggest that MAIT cells can discriminate and categorize complex human microbiota through computation of TCR signals depending on antigen load and presenting cells, and fine-tune their functional responses.
While this is in "Unrelated to ME/CFS research" forum, the blog below, from Jackson Labs, suggests that it could have some implication in ME.
https://jaxmecfs.com/2018/09/24/750/Jackson Labs ME/CFS Collaborative Center Director Derya Unutmaz and his collaborator and microbiome expert Julia Oh recently published a study in the journal Mucosal Immunology, titled “Tuning of human MAIT cell activation by commensal bacteria species and MR1-dependent T-cell presentation.” Mucosal-associated invariant T (MAIT) cells are a type of T cell present in various sites of the body, including the gut mucosa, and defend against microbial infection by recognizing a particular bacterial metabolite shown to them by antigen presenting cells (APCs). In the gut microbiota, there are many different species of bacteria present and yet, MAIT cells don’t mount an immune response to all of them. It is therefore likely that these cells can distinguish which types of bacteria are beneficial to us and which are harmful. The findings from this study could be highly relevant for ME/CFS patients, who are thought to have disruptions of both their immune system and their microbiome.