The background on this discovery is that in the course of my normal consulting, I had a cluster of 5 diet coaching clients over roughly one month presenting for a number of different goals, yet similar issues - with a common complaint of daytime fatigue.
Most had joint pains and involuntary muscle contractions. The male and female clients had endocrine, sleeping and neurological disorders, such as acute anxiety. The males and females exhibited signs of alopecia. All had extensive pathology data, spanning more than 10 years and a history of symptoms longer than 15 years. Only one client had ever been officially labeled as a "CFS/ME" patient.
I compiled and analyzed their pathology data and saw a common pattern of urea cycle abnormalities, cortisol / adrenal cortex dysregulation and mild leukopenia - specifically, borderline subclinical lymphocytes. ANA, CK, cRP, ESR, thyroid markers all unremarkable. Some minor liver enzyme elevations in some clients, which appeared to match their body composition and life choices. I thought the overall pattern was interesting, so I kept investigating.
Most clients had acute eating disorders. Ear/nose/throat infections were common. Environmental allergies were common. There was a history of GI issues and all had a specific pattern of food intolerances. Eggs and lecithin were consistently mentioned. I found that even more interesting.
I assessed their dietary habit using one of my favourite nutrition tracking tools, "Cronometer". The observed protein intake was very low - typically less than 40 grams per day, which did not match the unusual serum urea also being observed - BUN was typically high range, or in one client, very low range. This was interesting, because it suggested that either glutaminolysis was being used, and / or the urea cycle was impaired at different times.
3 of the clients had reported some benefits from ketogenic diets. 1 of them was currently employing a ketogenic diet. The others had not attempted this. This 1 client chose to discontinue their ketogenic diet and had an acute worsening of symptoms. This was interesting because it demonstrated a pattern of mitochondrial impairments.
All clients had a habitual lifestyle that obsessively revolved around dietary supplements. This was also interesting and it allowed me to ask them what supplements they took regularly and why.
Importantly, I also asked them what they didn't take and why - "what had they experienced negative reactions to?"
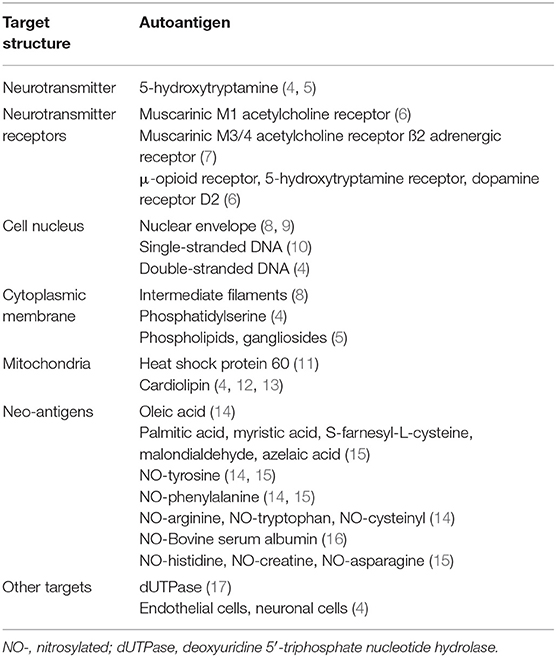
A common list of "problem" supplements for all clients was acetyl-l-carnitine, EGCG, choline, arginine, citrulline. Some of them reported that acetyl-l-carnitine caused acute edema and myopathy. I found that very interesting, also - suggesting influences to fatty acid oxidation / PDH, GDH, acetylcholine receptors, respectively.
All of the clients had exercise intolerance to even the mildest exertion levels, with suboptimal lactate threshold and oxygenation, even beyond my expectations for a sedentary lifestyle.
3 of the clients had prescriptions for salbutamol inhalers.
From this combined data, I saw more patterns forming. I analyzed other data they had captured, including HTMA tests, which excluded heavy metals, etc as a source of hypoxia.
At this point, I decided to take a personal interest in these cases and chose to work closely with 2 of these clients on a daily basis, exploring published literature and talking with them for typically 5-8 hours a day over many months, observing and analysing high levels of detail about their diet, daily activities, symptoms, influences / triggers / responses, while assembling connections between individual data points. This was a performed without any financial consideration. Being "retired" made this level of dedication and focus possible.
Dietary intervention of adding 2 eggs and some soy lecithin to every meal and 2 more before bed improved or resolved involuntary muscle spasms, with some not-unexpected discomforts. This was partially replaced by choline bitartate.
Pathology for Plasma Amino Acids found some common abnomalities with elevated glutamine, glutamic acid, low 1-methyl-histidine.
Exploring the literature and looking at the published CFS/ME metabolomics data, I saw many parallels between client data and published data. I explored this further, creating new connections along the way.
Serology markers showed high titre active EBV in both cases. There were differences in testing method availability, due to geographical location.
(Shared with full consent / expressed permissions.)
Client 1 -
EBV EBNA IgG++
EBV VCA IgG+++ (exceeded reporting thresholds)
EBV VCA IgM-
EBV EA was not provided
CMV IgG-
CMV IgM-
HSV-1++
HHV-6+
aPL-
AChR-MUSK-
Client 2 -
EBV EBNA was not provided
EBV VCA IgG++
EBV VCA IgM+
EBV EA was not provided
CMV IgG ++
CMV IgM -
aPL-
AChR-MUSK-
At this point, I considered that we had maybe progressed beyond "smoke", to "fire".
[QUESTION - "Perhaps the impact from lytic EBV infection or CMV was the source of the symptoms?"]
I reached out to those 2 clients' physicians and requested assistance. Under their care, off-label spironolactone (aldactone) was initiated at 25mg/day (Campo et al.) and client 1 increased to 2 x 25mg/day after 1 month. Client 2 also chose to self-administer nigella sativa for their CMV infection.
Over 3 months of close interactions, I observed many patterns in triggers / responses and durations, including associations between both clients' reported salbutamol usage vs timing of and cessation of upper-right abdominal pain, with increased energy levels.
The abdominal pain followed periods where they had been feeling better, with improved energy levels and decided to make use of them. Due to concomitant hypoxic symptoms, they self-administered salbutamol and this demonstrated a pattern of resolving their abdominal pain and also a reduction of the duration and intensity of post-exercise malaise. It also increased their energy levels. I found this very interesting.
The location of the pain and the relationship to the salbutamol dosage suggested strongly that beta-oxidation pathways were involved and the lactic acid cycle was impaired at hepatic gluconeogenesis. It didn't explain the cause of the high lactate, which I considered to be related to the impairments surrounding energy production.
Via close observation of client myopathy vs activity, I could see that unusual amounts of lactate were being generated, in addition to impairments in hepatic conversion back to glucose.
Combined with the noted urea cycle abnormalities and hypoxia, this was pointing strongly to a deficit in succinate and fumarate. The general lack of energy was suggesting an insufficient amount of ATP was being generated. This pointed to Complex V.
Gradually, over these months, I collected enough information from observations and literature searches to collectively create a hypothetical map.
Client 1 obtained a high result for EBV PCR roughly 1 month after starting spironolactone and flow cytometry, from the same sample showed low CD4. At 2 months, returned negative on PCR tests. WBC / flow cytometry all amazingly unremarkable.
Client 2 obtained negative results on both EBV and PCR test at roughly 6 weeks.
This was a strong suggestion that spironolactone has efficacy for arresting EBV, CMV lytic phase. Only expected side-effect being increased urination, requiring increased hydration and electrolytes.
Both clients had some tangible improvements to many symptoms, but were still showing all of the hallmark CFS/ME pattern of impairments I had personally experienced all those years ago.
[ANSWER - "The lytic phase is only partially responsible for CFS/ME. (n=2)"]
[QUESTION - "Wonderful, so what does this mean?"]
Looking at the pathway map I had created, three "hot-spots" were a-KGDH, PDH and selective beta-oxidation pathway insensitivity.
NutraEval reports are incredibly useful for identifying these abnormalities, however these need to be interpreted based on the level of activity prior to sampling, in much the same way that metabolomic studies need to be controlled against time of day and prior activity levels to provide any meaningful data.
Further to this, my research into the behaviour of HHV-infected cells revealed a metabolic preference for glutaminolysis (Krishna G et al), just like many cancer cells (Song Z et al.) and an ability to replicate via transcytosis (Hutt-Fletcher L et al.). This suggested a number of things, not the least of which was that these infected cells would be susceptible to the same metabolic influences as those cancer cells (Saunier E et al.). I considered that just like in certain types of cancer cells, the location and behaviour of the latent cells would have influence on the neighbouring cells. Where these are hepatic cells, this would unduly influence the hepatic function, in particular with regards to lactate metabolism / gluconeogenesis. In other tissues, many other disorders would be expected, where collagen synthesis and other tasks downstream of prolyl hydroxylase activities are degraded, leading to various states of inflammation and cortisol dysregulation.
As such, in my capacity as a diet and health coach, I educated Client 1 and Client 2 on the benefits of specific over-the-counter dietary supplements which are known for addressing these pathways, with advice to verify with their physician if contraindicated in their illnesses.
In the general population, like most dietary supplements in general, these specific dietary supplements would have little to no noticeable effects or benefits beyond those provided by a normal, balanced diet. They chose to purchase these from their local health food store or supplement vendor and self-administer them. They further chose to provide me with reports on their experiences with this self-experimentation.
Unlike the typical 'non-response' expected in the general population, the effects from these specific supplements were reported as both rapid and acute in both clients. Their energy levels returned to normal and they regained normal daily functionality and lifestyles. Due to their natural curiosity and a long history of experimentation with supplements, they also tried different combinations and dose schedules of these supplements and reported the effects. I analysed their reports and noticed a pattern, where failure to address any one of these "hot-spots" I had educated them on led to a consistently repeatable pattern of initial impairments and a resumption of full CFS/ME symptomology.
Using the combination of dietary supplments, viral EBNA IgG has been demonstrated to have decreased by 25% over 2 months, suggesting reduced systemic burden.
[ANSWER - "We are long past 'smoke', well past 'fire' and currently 'discussing the merits of different coloured fire extinguishers.'"]
[QUESTION - "This needs robust testing - how do I share this information with people who are in a better position to make use of it and without creating problems associated with communicating this around a demographic of patients who are desperate for early answers?"]
At this point, although having read perhaps 900 papers, I thought it would probably be best if I studied the literature further, wrote a review and shared it with the community. This presented some new difficulties, as although demonstrated by my recent manuscript, through personal interests my understanding of metabolism, rheumatology, cellular biology, immunology, endocrinology and biological pathways could be considered with some equivalencies to a PhD level education, due to my life choices and preference for self-education, usually by intense reading, I lack the credentials required to present these findings to a wider audience, in the format they would normally be inclined to appreciate and give due consideration.
I prefer to learn things in my own way and explore topics in an organic way, where my brain absorbs them efficently. I find structured education traditionally 'grinds my gears' by causing frustrations and inefficiencies, therefore I limit any formal education and certifications to the barest minimum required to permit me to work in any specific field. This is also likely why I left school at 14 and "retired" at 38. Overall, I have lived an unusual life.
A self-taught "diet and health coach" traditionally does not write medical journal articles on complex metabolic disorders and virology. This is a significant anomaly, although my life to-date has been one long anomaly. Importantly, I also lacked a full understanding of the nuances and expectations of academia, with regards to publishing material for peer-review.
[ANSWER - "Fortunately, through fate and/or luck, my life-partner and co-author happens to be a brilliant scientist, holding a PhD in Neuroimmunology, with a Masters in Biochemistry. Keeping in line with my usual preference for organic learning, she helped me understand the normal requirements for publishing a paper, assisted and answered questions about lab methodology, where I found criticisms of papers I was reading, edited and helped proof the manuscript, along with many other key aspects of the journey towards where we are today. I'm always thankful for having her in my life." ]
In the process of continuing to map the pathophysiology, draw the diagrams and write the paper, my research connected the dots with a broader array of disorders and diseases. I realised that my research had significantly greater implications for many diseases and disorders. During the many weeks that was required to author the paper, I was was also contacted by some other clients and friends who had a number of different diseases / disorders - including bipolar disorder, schizophrenia, ehlers danlos syndrome, lupus and rheumatoid arthritis, which were already strongly hinted at having a common origin, by the growing manuscript and diagrams.
Consequently, I found the same signature of metabolic alterations and serology markers in those clients and they show an acute response to the same dietary supplement advice, although there are variations and further optimisations possible where hepatic impairment cannot be demonstrated or where lytic phase cannot be detected in serology. For each of these disease model sub-types, I have drafted early specifications that can be used for testing in clinical trial research around these disorders. In CFS/ME or hepatic infection, there are currently known limitations, preventing a perfect solution. There are two small mitochondrial "leaks" to resolve regarding a-KG accumulation and ROS. They're manageable and still provide a treatment which allows normal daily life, however this can be further improved.
This is where we need help in continuing this journey.
[QUESTION - "Can you please assist?"]