ukxmrv
Senior Member (Voting Rights)
There were UK and Australian clinics drugging various patientsWhen I was in a bad crash I wondered to myself if someone could put me in an induced coma for a while to let me not have to experience the crash. Purely hypothetical of course.
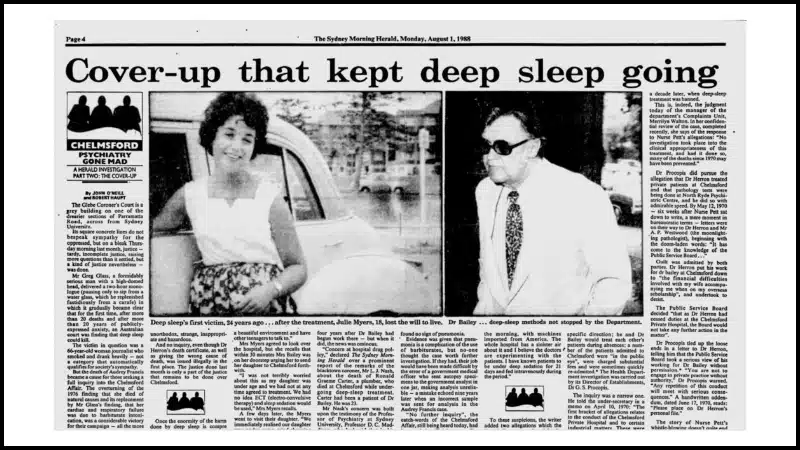
Chelmsford deep sleep therapy: Exposing systemic failings that denied justice
We represented the victims of lethal ‘Deep Sleep Therapy’ at Chelmsford Hospital.

William Sargant - Wikipedia
This doctor was 'treating' ME patients and tried to get me into his private one in London
Preying on Hope | DuncanCampbell.org
The ME patients I met or spoke with who had seen him were all worse. One went from his clinic into a psych hospital.
Last edited:

