John Mac
Senior Member (Voting Rights)
Abstract
Background/Objectives: Orthostatic intolerance is prevalent in patients with myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) and is caused by an abnormal reduction in cerebral blood flow (CBF). In healthy controls (HCs), CBF is regulated complexly, and cardiac output (CO) is an important determinant of CBF. A review in HC showed that a 30% reduction in CO results in a 10% reduction in CBF. In contrast, we showed in ME/CFS patients with a normal HR (HR) and blood pressure response during a tilt test that CO and CBF decreased to a similar extent. The relation between CO and CBF in ME/CFS patients with postural orthostatic tachycardia syndrome (POTS) is unknown. Therefore, the aim of this study is to assess the relation between CBF and CO, in ME/CFS patients with POTS.
The methods used in this retrospective study analyze this relation in a large group of patients. We also analyzed the influence of clinical data. A total of 260 ME/CFS patients with POTS underwent tilt testing with measurements of HR, BP, CBF, CO, and end-tidal PCO2. We measured CBF using extracranial Doppler flow velocity and vessel diameters obtained with a General Electric echo system, and suprasternal aortic flow velocities were measured using the same device. We recorded end-tidal PCO2 using a Nonin Lifesense device.
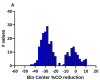
Results: End-tilt HR and the HR increase were significantly higher in the patients with a %CO reduction ≥ −15% than in the other group. End-tilt CO was higher and the %CO reduction was lower in patients with %CO reduction ≥ −15% than in the other group. CBF data (supine, end-tilt and the %CBF reduction) were not different between the two patient groups. The use of HR increases and %SV reductions were not as discriminative as the %CO reduction.
Conclusions: In ME/CFS patients with POTS during tilt testing with measurements of both the CO and the CBF, two different patterns were observed: (1) appr. two-thirds of patients had an almost 1:1 relation between the %CBF reduction and the %CO reduction. (2) Appr. one-third of patients showed a limited reduction in CO together with a substantial increase in HR. In these patients, there was no relation between the CO and CBF reduction. These data suggest the presence of a hyperadrenergic response.
https://www.mdpi.com/2077-0383/14/11/3648
Background/Objectives: Orthostatic intolerance is prevalent in patients with myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) and is caused by an abnormal reduction in cerebral blood flow (CBF). In healthy controls (HCs), CBF is regulated complexly, and cardiac output (CO) is an important determinant of CBF. A review in HC showed that a 30% reduction in CO results in a 10% reduction in CBF. In contrast, we showed in ME/CFS patients with a normal HR (HR) and blood pressure response during a tilt test that CO and CBF decreased to a similar extent. The relation between CO and CBF in ME/CFS patients with postural orthostatic tachycardia syndrome (POTS) is unknown. Therefore, the aim of this study is to assess the relation between CBF and CO, in ME/CFS patients with POTS.
The methods used in this retrospective study analyze this relation in a large group of patients. We also analyzed the influence of clinical data. A total of 260 ME/CFS patients with POTS underwent tilt testing with measurements of HR, BP, CBF, CO, and end-tidal PCO2. We measured CBF using extracranial Doppler flow velocity and vessel diameters obtained with a General Electric echo system, and suprasternal aortic flow velocities were measured using the same device. We recorded end-tidal PCO2 using a Nonin Lifesense device.
Results: End-tilt HR and the HR increase were significantly higher in the patients with a %CO reduction ≥ −15% than in the other group. End-tilt CO was higher and the %CO reduction was lower in patients with %CO reduction ≥ −15% than in the other group. CBF data (supine, end-tilt and the %CBF reduction) were not different between the two patient groups. The use of HR increases and %SV reductions were not as discriminative as the %CO reduction.
Conclusions: In ME/CFS patients with POTS during tilt testing with measurements of both the CO and the CBF, two different patterns were observed: (1) appr. two-thirds of patients had an almost 1:1 relation between the %CBF reduction and the %CO reduction. (2) Appr. one-third of patients showed a limited reduction in CO together with a substantial increase in HR. In these patients, there was no relation between the CO and CBF reduction. These data suggest the presence of a hyperadrenergic response.
https://www.mdpi.com/2077-0383/14/11/3648