You are using an out of date browser. It may not display this or other websites correctly.
You should upgrade or use an alternative browser.
You should upgrade or use an alternative browser.
Trial Report Resistance Exercise Therapy for Long COVID: a Randomized, Controlled Trial 2025 Berry et al.
- Thread starter ME/CFS Science Blog
- Start date
Someone added a comment to the paper (scroll to the bottom):
Misleading interpretation of the null results?
First paragraph:
In the Statistical Analysis plan, the authors state that "[t]he minimum clinically important between-group difference in the ISWT at follow-up (3 months) = 46 m, SD=105 [20]." The adjusted mean difference between the groups was 36.5 m, well below the threshold of MCID.
Authors responded:
We appreciate the interest in the CISCO-21 trial of resistance exercise in people after COVID-19 infection. In this trial, a personalized program of resistance exercise for 3-months improved walking capacity, health-related quality of life and hand grip strength and was well tolerated. A broad range of secondary outcomes were assessed but the trial was not powered for secondary outcome analyses. The enrolled population was not frail therefore, expectedly, perception of frailty did not improve.
We agree that in an open-label trial, participant responses are susceptible to expectation bias, but there is no evidence for or against bias in this study.
On the other hand, there is evidence of benefit. The primary outcome was met and this was associated with an improvement in health-related quality of life.
We disagree that the observed improvements in secondary outcomes are small; the magnitude of improvement in grip strength (2.6 kg) is meaningful and this assertion is supported by the literature.
There are few, if any, evidence-based therapies for post-COVID-19 conditions. Based on the results of the CISCO-21 trial, resistance exercise is safe, inexpensive and effective for improving physical function in people after COVID-19 infection. Resistance exercise is accessible to a broad range of individuals. This study supports adoption of personalised resistance exercise as a therapy option for people with post-COVID-19 conditions.
They didn't say anything about the commenter's main point - that the pre-selected minimum important difference was not achieved.
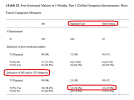
eyes also on indication of PEM (above top circled area) - PEM needs better definition?Eyes on eTable 28 everybody:
View attachment 29333
rvallee
Senior Member (Voting Rights)
It's hard to not see academia as being totally broken when this is so completely routine the journals don't even care. All they do is repeat the marketing bullet points and ignore every single point of criticism. Obviously the academics don't care either, which is basically a red flag whose fibres are themselves made entirely of red flags.Authors responded:
They didn't say anything about the commenter's main point - that the pre-selected minimum important difference was not achieved.
Actually this isn't just routine, in evidence-based rehab it's almost universal. Every step of the research stage is useless at preventing fraud and pseudoscientific ideology. Peer review editorial review are just as useless, as long as they get the payments they don't care. Post-publication comments don't even matter, they can simply do the equivalent of saying "but Red Bull gives you wiiiiings" and it's all good to everyone involved, except the tiny few of us who actually care because we have all the stakes.
Those systems have become so bad it's actually hard to see any reason to keep propping them up. Science and expertise have been targets of illegitimate attacks, but have become so complacent and corrupt all on their own that it's actually hard to defend the value of this system, it has clearly passed the limits of what it can achieve. Their own mistakes create too much distraction to even focus on the illegitimate attacks, but those systems are totally incapable of fixing themselves.
Utsikt
Senior Member (Voting Rights)
Getting caught in a lie and doubling down.. Classic propaganda.It's hard to not see academia as being totally broken when this is so completely routine the journals don't even care. All they do is repeat the marketing bullet points and ignore every single point of criticism. Obviously the academics don't care either, which is basically a red flag whose fibres are themselves made entirely of red flags.
Actually this isn't just routine, in evidence-based rehab it's almost universal. Every step of the research stage is useless at preventing fraud and pseudoscientific ideology. Peer review editorial review are just as useless, as long as they get the payments they don't care. Post-publication comments don't even matter, they can simply do the equivalent of saying "but Red Bull gives you wiiiiings" and it's all good to everyone involved, except the tiny few of us who actually care because we have all the stakes.
Those systems have become so bad it's actually hard to see any reason to keep propping them up. Science and expertise have been targets of illegitimate attacks, but have become so complacent and corrupt all on their own that it's actually hard to defend the value of this system, it has clearly passed the limits of what it can achieve. Their own mistakes create too much distraction to even focus on the illegitimate attacks, but those systems are totally incapable of fixing themselves.
Karen Kirke
Senior Member (Voting Rights)
In the next few posts, I am sharing youtube links for the exercises participants did in this study, with permission from Prof Stuart Gray, who was in charge of the exercise intervention.
In each case, participants did the upper body exercises from the start, and added in lower body exercises from week 3.
Three exercise categories and guidance were provided according to the status of the participant:
(1) confined to bed…
(2) able to sit up…
(3) ambulatory…
In each case, participants did the upper body exercises from the start, and added in lower body exercises from week 3.
Last edited:
Karen Kirke
Senior Member (Voting Rights)
Confined to bed
Upper body exercises
Lying chest-press
Lying row
Lower body exercises
Lying toe points
Lying leg press
Bridging
Shared with permission from Prof Stuart Gray, who was in charge of the exercise intervention.
Upper body exercises
Lying chest-press
Lying row
Lower body exercises
Lying toe points
Lying leg press
Bridging
Shared with permission from Prof Stuart Gray, who was in charge of the exercise intervention.
Last edited:
Karen Kirke
Senior Member (Voting Rights)
Able to sit up
Upper body exercises
Seated chest-press
Seated row (no video)
Seated arm raises
Chest stretches (no video)
Lower body exercises
Seated leg extensions
Seated toe pointing
Squats (no video)
Shared with permission from Prof Stuart Gray, who was in charge of the exercise intervention.
Upper body exercises
Seated chest-press
Seated row (no video)
Seated arm raises
Chest stretches (no video)
Lower body exercises
Seated leg extensions
Seated toe pointing
Squats (no video)
Shared with permission from Prof Stuart Gray, who was in charge of the exercise intervention.
Last edited:
Karen Kirke
Senior Member (Voting Rights)
Ambulatory
Upper body exercises
Press-ups
Standing arm raises
Seated rows
Chest stretches (no video)
Lower body exercises
Lunges
Calf raises
Shared with permission from Prof Stuart Gray, who was in charge of the exercise intervention.
Upper body exercises
Press-ups
Standing arm raises
Seated rows
Chest stretches (no video)
Lower body exercises
Lunges
Calf raises
Shared with permission from Prof Stuart Gray, who was in charge of the exercise intervention.
Last edited:
Karen Kirke
Senior Member (Voting Rights)
A study author sent me a draft manual for the exercise intervention in this study. It’s by Gray, Boiskin & Berry and is dated February 2021. I don’t have permission to share it, but I do have permission to summarise it and quote from it.
I’ll summarise it in terms of what’s similar and different between the manual by Gray, Boiskin & Berry 2021 and exercise manuals we’re familiar with from the PACE and GETSET trials.
Similarities
At 39 pages, the manual by Gray, Boiskin & Berry 2021 is about the same length as the GETSET participant booklet, and considerably shorter than the PACE GET manual (110 pages of text plus forms taking it to 142 pages).
As in the GETSET manual’s section on stretching, the strengthening exercises are described in both words and pictures in the manual by Gray, Boiskin & Berry 2021. GBB also provide youtube links (see posts above).
Differences
PACE & GETSET manuals emphasize the importance of starting from a stabilised baseline. The manual by Gray, Boiskin & Berry 2021 does not mention stabilising or a baseline.
Both PACE and GETSET manuals are primarily geared towards activities like walking, whereas the exercises in Gray, Boiskin & Berry 2021 are all strengthening exercises.
Both PACE and GETSET manuals spend a lot of time on the theory behind GET in ME/CFS, and models of ME/CFS. This is particularly true of the PACE manual. The manual by Gray, Boiskin & Berry 2021, by contrast, explains the rationale for their study in a few simple sentences:
When you read the Gray, Boiskin & Berry 2021 manual, you don’t get a hard sell like you do with the PACE and GETSET manuals. There’s one page where they expound on the benefits of exercise, and that’s it:
The most notable difference is in what the manuals recommend to do if you feel bad.
Gray, Boiskin & Berry 2021:
Contrast this with the GETSET and PACE GET manuals, both of which make a distinction between what you should do if you’re feeling bad because of an infection (reduce activity) and what you should do if you’re feeling bad because of ME/CFS (maintain activity), and then go to some lengths to convince the patient why they should maintain activity despite feeling worse:
GETSET participant booklet:
PACE GET participant manual:
I’ll summarise it in terms of what’s similar and different between the manual by Gray, Boiskin & Berry 2021 and exercise manuals we’re familiar with from the PACE and GETSET trials.
Similarities
At 39 pages, the manual by Gray, Boiskin & Berry 2021 is about the same length as the GETSET participant booklet, and considerably shorter than the PACE GET manual (110 pages of text plus forms taking it to 142 pages).
As in the GETSET manual’s section on stretching, the strengthening exercises are described in both words and pictures in the manual by Gray, Boiskin & Berry 2021. GBB also provide youtube links (see posts above).
Differences
PACE & GETSET manuals emphasize the importance of starting from a stabilised baseline. The manual by Gray, Boiskin & Berry 2021 does not mention stabilising or a baseline.
Both PACE and GETSET manuals are primarily geared towards activities like walking, whereas the exercises in Gray, Boiskin & Berry 2021 are all strengthening exercises.
Both PACE and GETSET manuals spend a lot of time on the theory behind GET in ME/CFS, and models of ME/CFS. This is particularly true of the PACE manual. The manual by Gray, Boiskin & Berry 2021, by contrast, explains the rationale for their study in a few simple sentences:
We led a successful clinical research study based in the West of Scotland. We found that some patients had reduced exercise capacity. We now propose a study of a new treatment (muscle strengthening exercise) that is suitable for patients of all ages and health backgrounds.
When you read the Gray, Boiskin & Berry 2021 manual, you don’t get a hard sell like you do with the PACE and GETSET manuals. There’s one page where they expound on the benefits of exercise, and that’s it:
Benefits of exercise
We invite you to perform muscle strengthening exercises daily for the duration of the study. Patients who have suffered from COVID-19 can have longer term issues such as chest pain, breathlessness and fatigue. COVID-19 can reduce muscle function, particularly people who were in the intensive care unit. In fact, only 2 weeks of reduced physical activity can reduce around 5% of the muscle in your legs. COVID-19 can also affect the function of the muscle that help you breathe.
Exercise can help to reduce chest pain, breathlessness and fatigue in many conditions. Muscle strengthening exercise can help to increase the size of your muscles and their function. This is on top of the many wider health benefits of exercise. We aim to test the effects of a muscle strengthening programme in people who have suffered from COVID-19.
The most notable difference is in what the manuals recommend to do if you feel bad.
Gray, Boiskin & Berry 2021:
Don’t over do it!
If you find that you are feeling very fatigued on any days then don’t push yourself too hard, it is ok to take a day off from the exercises every now and then. Also whilst we will encourage you to progress and make the exercises a bit harder over time we don’t want you to try exercises you are not ready for. So don’t try to push and progress to more difficult exercises when these are too challenging for you.
Contrast this with the GETSET and PACE GET manuals, both of which make a distinction between what you should do if you’re feeling bad because of an infection (reduce activity) and what you should do if you’re feeling bad because of ME/CFS (maintain activity), and then go to some lengths to convince the patient why they should maintain activity despite feeling worse:
GETSET participant booklet:
If your setback is CFS/ME related then you should try and continue exercising at your current level to the best of your ability. It is often incorrectly assumed that an increase in symptoms equals harm. It doesn’t. If you continue at the exercise level you are on now you may well find that you feel no worse, and after a short while you may actually feel better. Remember that although you may not feel like exercising during a CFS/ME related setback, by resting too much you can quickly lose the physical gains that you have made.
Setbacks are a normal part of recovery and so it is important to remain as positive as possible. As you get stronger you will find that you have fewer setbacks and they are less severe and last a shorter time
• Try to maintain as much physical activity as you can even if this seems difficult.
• Resting too much will probably worsen your condition in the long run. Even resting for a week can make it much harder to get back to where you were on the GET programme.
• If you cannot do your exercise in one go break it into two or more sessions.
• If you have had to stop an activity or an exercise get back to it as soon as you can.
PACE GET participant manual:
Dealing with a CFS/ME setback: what should I do?
During a CFE/ME setback, it is understandable that you might wish to rest and reduce the amount of activity you do, because you don’t feel well and activity feels much harder than usual. This may even be a time in which you become concerned that the increase in symptoms may be causing you damage.
The evidence we have is in fact the opposite: there is no evidence to suggest that an increase in symptoms is causing you harm. It is certainly uncomfortable and unpleasant, but not harmful. In fact, there is much evidence to support the alternate view: if you rest too much, it is the resting that can cause negative changes in the body. Resting and withdrawing from activity can also make us feel fed up or worried, and this can also make it harder to continue being active.
The periods of excessive rest can be a time when the body adjusts to the lower level of activity and weakens: if the body weakens further, it can become more sensitive to activity and make overall symptoms worse.
Last edited:
Utsikt
Senior Member (Voting Rights)
Thank you for sharing @Karen Kirke
I think the quotes from the manual completely misses the mark.
There is no documentation that the lack of exercise (or physical activity in general) is the cause of the symptoms they mention, and there is no justification for why introducing exercises would help in this population.
This is akin to a doctor giving a COPD or lung cancer patients cough syrup because they are coughing.
Speaking from personal experience as someone that’s been bedbound for more than a year, doing leg presses or bridges would eat up a substantial percentage of my daily physical capacity. It would be the difference between being able to use the toilet whenever I need to, and having to lie and wait for hours because me legs need more rest before I use them again. Doing the arm exercises would reduce my ability to independently take care of my personal hygiene.
It would eradicate whatever buffer I have left to the point that I would not be able to fetch important items I need (e.g. essential medications or my phone to contact help) if I forgot to bring them with me when moving between the night and day beds I use that are five meters apart.
Edit: safely doing X without risking PEM or substantial immediate symptoms.
I think the quotes from the manual completely misses the mark.
There is no documentation that the lack of exercise (or physical activity in general) is the cause of the symptoms they mention, and there is no justification for why introducing exercises would help in this population.
This is akin to a doctor giving a COPD or lung cancer patients cough syrup because they are coughing.
Speaking from personal experience as someone that’s been bedbound for more than a year, doing leg presses or bridges would eat up a substantial percentage of my daily physical capacity. It would be the difference between being able to use the toilet whenever I need to, and having to lie and wait for hours because me legs need more rest before I use them again. Doing the arm exercises would reduce my ability to independently take care of my personal hygiene.
It would eradicate whatever buffer I have left to the point that I would not be able to fetch important items I need (e.g. essential medications or my phone to contact help) if I forgot to bring them with me when moving between the night and day beds I use that are five meters apart.
Edit: safely doing X without risking PEM or substantial immediate symptoms.
Last edited:
NelliePledge
Senior Member (Voting Rights)
Apologies for not having read all the details. I always come back on anything that is recommending people do any type of exercise to my basic question. If I had the capacity to do these exercises why wouldn’t I use that on doing something I have on my long list of things I need or want to do that actually have a practical purpose or social benefit.
For context as someone with moderate severity ME my daily living activities I put away all my own groceries, I do all my own clothes washing, I empty and fill my own dishwasher and put everything back in the cupboards. I prepare my own food. When I can I have a fire in my log burner. All these things already require me to move and lift stuff. If I do extra stuff I have to cut back on these daily living activities.
For context as someone with moderate severity ME my daily living activities I put away all my own groceries, I do all my own clothes washing, I empty and fill my own dishwasher and put everything back in the cupboards. I prepare my own food. When I can I have a fire in my log burner. All these things already require me to move and lift stuff. If I do extra stuff I have to cut back on these daily living activities.
Karen Kirke
Senior Member (Voting Rights)
If I've understood correctly, they found that the resistance exercise intervention did not help chest pain, breathlessness or fatigue more than standard care (which included access to rehabilitation).There is no documentation that the lack of exercise (or physical activity in general) is the cause of the symptoms they mention, and there is no justification for why introducing exercises would help in this population.
So if you had been in the intervention arm of the study, you would probably have withdrawn, like 17 of the intervention group (vs 9 of the control group), or you would have been in the 7.6% who did not adhere ≥ 10%:Speaking from personal experience as someone that’s been bedbound for more than a year, doing leg presses or bridges would eat up a substantial percentage of my daily physical capacity. It would be the difference between being able to use the toilet whenever I need to, and having to lie and wait for hours because me legs need more rest before I use them again. Doing the arm exercises would reduce my ability to independently take care of my personal hygiene.
It would eradicate whatever buffer I have left to the point that I would not be able to fetch important items I need (e.g. essential medications or my phone to contact help) if I forgot to bring them with me when moving between the night and day beds I use that are five meters apart.
In the GETSET trial:
The physiotherapists reported that 43 participants (42%) adhered to GES completely or very well, 31 (30%) moderately well, and 30 (29%) slightly or not at all.
Karen Kirke
Senior Member (Voting Rights)
Yeah, the usual argument put forward is that by doing exercise you would be able to do more of those things that have a practical purpose or social benefit, but that doesn't seem to pan out for us, does it? I remember well what it was like when exercise had that effect - it was great, like a cure-all.Apologies for not having read all the details. I always come back on anything that is recommending people do any type of exercise to my basic question. If I had the capacity to do these exercises why wouldn’t I use that on doing something I have on my long list of things I need or want to do that actually have a practical purpose or social benefit.
For context as someone with moderate severity ME my daily living activities I put away all my own groceries, I do all my own clothes washing, I empty and fill my own dishwasher and put everything back in the cupboards. I prepare my own food. When I can I have a fire in my log burner. All these things already require me to move and lift stuff. If I do extra stuff I have to cut back on these daily living activities.
Utsikt
Senior Member (Voting Rights)
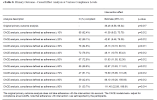
It didn’t help for anything at all. Every single outcome was either not statistical significant and/or clinically meaningful, or at an unacceptably high risk of bias.If I've understood correctly, they found that the resistance exercise intervention did not help chest pain, breathlessness or fatigue more than standard care (which included access to rehabilitation).
But my point was that there was no evidence for their theory or interventions before the trial. The rationale to do it just wasn’t there.
I would never have participated in the first place. Very few people in my position are willing to sign up to trials like these.So if you had been in the intervention arm of the study, you would probably have withdrawn, like 17 of the intervention group (vs 9 of the control group), or you would have been in the 7.6% who did not adhere ≥ 10%:
Karen Kirke
Senior Member (Voting Rights)
But my point was that there was no evidence for their theory or interventions before the trial. The rationale to do it just wasn’t there.
I'm not clear on which part of their rationale you don't agree with, because you don't need lack of X to be the cause of Y in order for X to improve Y - think of rehabilitation in an area like stroke where there's good evidence of benefit. Which bit of their rationale do you object to:There is no documentation that the lack of exercise (or physical activity in general) is the cause of the symptoms they mention, and there is no justification for why introducing exercises would help in this population.
The Incremental ShuttleWalk Test is an established measure of functional capacity for rehabilitation among people with respiratory disease. Muscle strength is a determinant of Incremental ShuttleWalk Test performance,39 and a decrease in muscle strength after COVID-19 is associated with decreased Incremental ShuttleWalk Test performance.40 Muscle strength may be impaired after COVID-1941; hence, muscle strength after COVID-19 represented a target for the resistance exercise intervention in this trial, with the overall aim of improving functional capacity. For these reasons, our trial tested resistance exercise as a method to improve Incremental ShuttleWalk Test performance. Prior mechanistic studies indicate that resistance exercise interventions may enhance muscle strength and aerobic fitness,42,43 which are determinants of functional capacity. The mechanisms may involve improvements in type II muscle fiber recruitment,44 flow-mediated vasodilatation,45 and ventricular stroke volume.46-48 There are other clinical trials of exercise interventions in long COVID,11,49,50 and the design and results of our trial in relation to these prior studies are discussed in the eDiscussion in Supplement 2.
Karen Kirke
Senior Member (Voting Rights)
It would be interesting to know what the percentages were at baseline.Eyes on eTable 28 everybody:
View attachment 29333
Thank you for the videos, @Karen Kirke.
What do they expect people to do who are already operating at their PEM threshold just to get through the necessary activities to stay fed and clean? I had a look through the exercises for ambulatory, since I can walk in my home, though I spend most of my time lying down and am only able, for example, to shower about once a week and do little or nothing else that day.
Does it say how many repetitions they asked people to do for each exercise?
This seems totally impractical for most of us. As others have said, why do an arm raising exercise when you already raise your arms to put things in cupboards or wash your hair. And so on. If I tried to add these to my day I would crash.
Even if I had capacity by cutting back other things in order to do the exercises, I might get a bit stronger, but would still be just a sick.
What do they expect people to do who are already operating at their PEM threshold just to get through the necessary activities to stay fed and clean? I had a look through the exercises for ambulatory, since I can walk in my home, though I spend most of my time lying down and am only able, for example, to shower about once a week and do little or nothing else that day.
Does it say how many repetitions they asked people to do for each exercise?
This seems totally impractical for most of us. As others have said, why do an arm raising exercise when you already raise your arms to put things in cupboards or wash your hair. And so on. If I tried to add these to my day I would crash.
Even if I had capacity by cutting back other things in order to do the exercises, I might get a bit stronger, but would still be just a sick.
Utsikt
Senior Member (Voting Rights)
I'm not clear on which part of their rationale you don't agree with, because you don't need lack of X to be the cause of Y in order for X to improve Y - think of rehabilitation in an area like stroke where there's good evidence of benefit. Which bit of their rationale do you object to:
LC in general is not like a respiratory disease. The post ICU-patients might have some similarities, bit the post-mild infection patients don’t. They recruited everyone with pretty much any symptoms.The Incremental ShuttleWalk Test is an established measure of functional capacity for rehabilitation among people with respiratory disease.
But they were talking about respiratory disease, which would imply impaired oxygen extraction in the lungs, not weakened muscles.Muscle strength is a determinant of Incremental ShuttleWalk Test performance,39
Association does not imply causation. Loss of taste and smell is probably also somewhat associated with decrease ISWT performance. Do they think that smell training might improve ISWT performance as well?and a decrease in muscle strength after COVID-19 is associated with decreased Incremental ShuttleWalk Test performance.40
Only if muscle strength is the limiting factor for functional capacity. They have not made any reasonable arguments for that being the case in these patients.Muscle strength may be impaired after COVID-1941; hence, muscle strength after COVID-19 represented a target for the resistance exercise intervention in this trial, with the overall aim of improving functional capacity.
So for no reason at all, then.For these reasons, our trial tested resistance exercise as a method to improve Incremental ShuttleWalk Test performance.
As above.Prior mechanistic studies indicate that resistance exercise interventions may enhance muscle strength and aerobic fitness,42,43 which are determinants of functional capacity.
42 is a review where the quality of the evidence was low or very low - like every CBT and GET trial NICE rejected in NG206.
43 is a review from 1998 about exercise for heart failure patients. Not comparable.
11 is a meta review of studies with pretty poor risk of bias ratings:The mechanisms may involve improvements in type II muscle fiber recruitment,44 flow-mediated vasodilatation,45 and ventricular stroke volume.46-48 There are other clinical trials of exercise interventions in long COVID,11,49,50 and the design and results of our trial in relation to these prior studies are discussed in the eDiscussion in Supplement 2.
49 does not look like it was a good study:
50 had null results:
——
Do you think any of these claims hold up under scrutiny?
rvallee
Senior Member (Voting Rights)
I have done almost all of that. None of it helped. I actually made myself significantly worse because even that little was too much. I needed for my functioning to improve before I could do more than the barest minimum, and no amount of doing so made any difference other than muscular. It slightly reduces aches and pains, and not much more.
The whole thing is laughable. No one without a serious pathology needs anything remotely like this. This is the kind of protocol that would take someone from a long coma to normal functioning, except it would probably take just a few months, whereas in ME/CFS this could applied every single day for years and make zero difference.
This is all just completely unserious. Junk nonsense like this would be mocked mercilessly if medicine wasn't so dysfunctional, but we are years into the merger of real and alternative medicine, and pointing out the emperor's ass pimple is simply not allowed.
The whole thing is laughable. No one without a serious pathology needs anything remotely like this. This is the kind of protocol that would take someone from a long coma to normal functioning, except it would probably take just a few months, whereas in ME/CFS this could applied every single day for years and make zero difference.
This is all just completely unserious. Junk nonsense like this would be mocked mercilessly if medicine wasn't so dysfunctional, but we are years into the merger of real and alternative medicine, and pointing out the emperor's ass pimple is simply not allowed.