ME/CFS Science Blog
Senior Member (Voting Rights)
Abstract
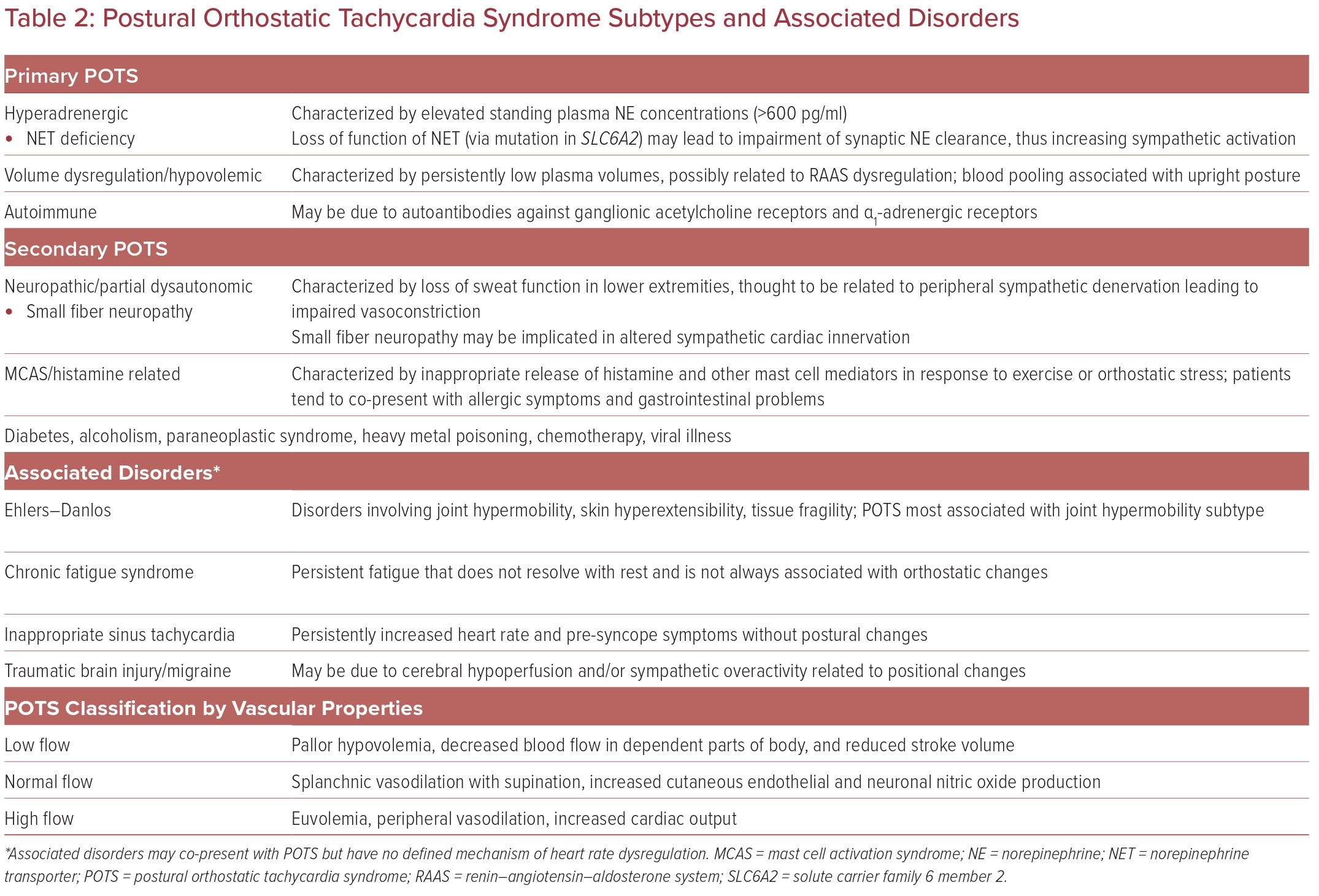
Although diagnostic criteria have been developed characterizing postural orthostatic tachycardia syndrome (POTS), no single set of criteria is universally accepted. Furthermore, there are gaps in the present criteria used to identify individuals who have this condition. The reproducibility of the physiological findings, the relationship of symptoms to physiological findings, the presence of symptoms alone without any physiological findings and the response to various interventions confuse rather than clarify this condition. As many disease entities can be confused with POTS, it becomes critical to identify what this syndrome is. What appears to be POTS may be an underlying condition that requires specific therapy. POTS is not simply orthostatic intolerance and symptoms or intermittent orthostatic tachycardia but the syndrome needs to be characterized over time and with reproducibility. Here we address critical issues regarding the pathophysiology and diagnosis of POTS in an attempt to arrive at a rational approach to categorize the syndrome with the hope that it may help both better identify individuals and better understand approaches to therapy.
https://pubmed.ncbi.nlm.nih.gov/32222376/
Although diagnostic criteria have been developed characterizing postural orthostatic tachycardia syndrome (POTS), no single set of criteria is universally accepted. Furthermore, there are gaps in the present criteria used to identify individuals who have this condition. The reproducibility of the physiological findings, the relationship of symptoms to physiological findings, the presence of symptoms alone without any physiological findings and the response to various interventions confuse rather than clarify this condition. As many disease entities can be confused with POTS, it becomes critical to identify what this syndrome is. What appears to be POTS may be an underlying condition that requires specific therapy. POTS is not simply orthostatic intolerance and symptoms or intermittent orthostatic tachycardia but the syndrome needs to be characterized over time and with reproducibility. Here we address critical issues regarding the pathophysiology and diagnosis of POTS in an attempt to arrive at a rational approach to categorize the syndrome with the hope that it may help both better identify individuals and better understand approaches to therapy.
https://pubmed.ncbi.nlm.nih.gov/32222376/