You are using an out of date browser. It may not display this or other websites correctly.
You should upgrade or use an alternative browser.
You should upgrade or use an alternative browser.
Long Covid in the media and social media 2023
- Thread starter rvallee
- Start date
- Status
- Not open for further replies.
Sly Saint
Senior Member (Voting Rights)
Long Covid Families
@LongCovidFam
Many #LongCovidKids had mild or asymptomatic cases of acute Covid. Developed #longcovid around month 2/3. Felt better around month 5 only to contract a serious case of #RSV or #FLU which worsen LC symptoms and caused further disability. 1/
Last edited:
rvallee
Senior Member (Voting Rights)
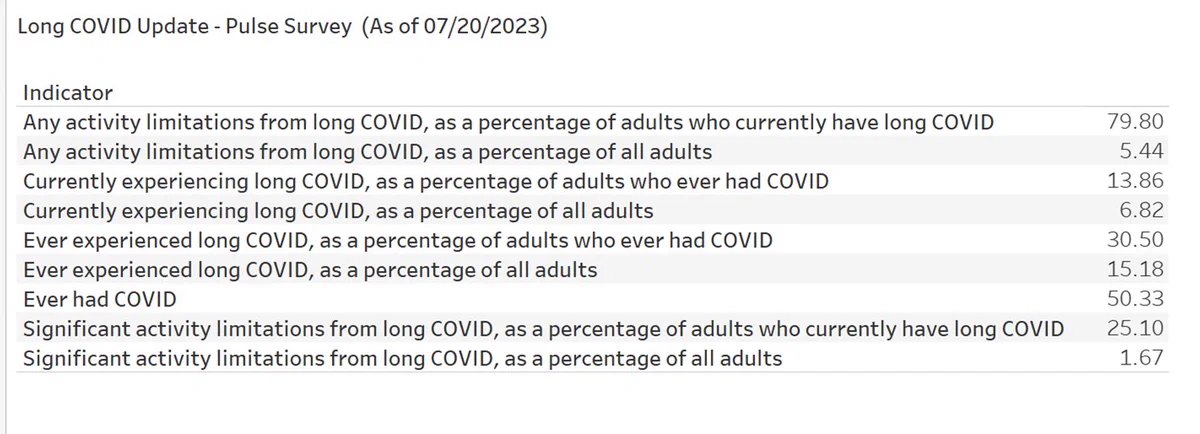
Latest CDC data (July 20) show an increase in Long Covid, with about 1/4 having significant limitations. Unless I misremember it, a UK survey found a similar increase.
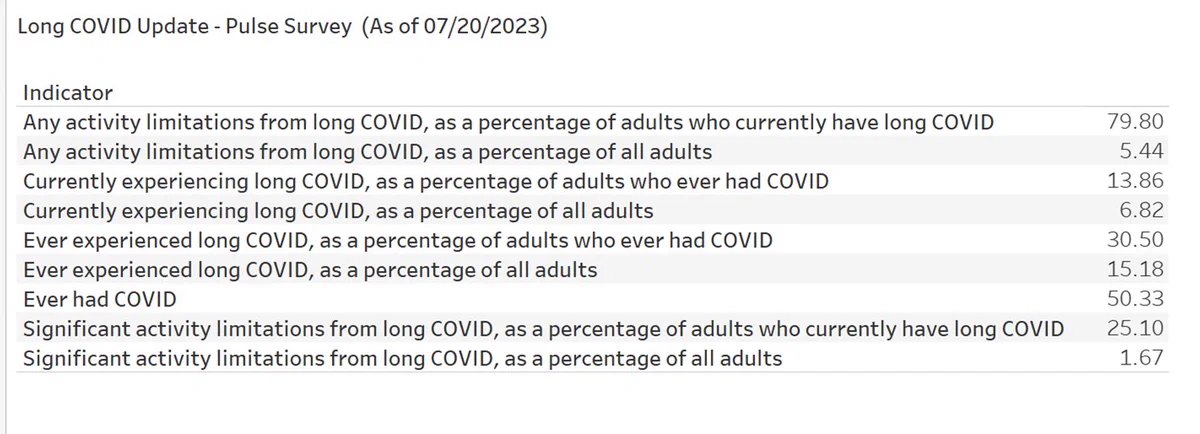
https://data.cdc.gov/NCHS/Post-COVID-Conditions/gsea-w83j
https://data.cdc.gov/NCHS/Post-COVID-Conditions/gsea-w83j
rvallee
Senior Member (Voting Rights)
The business press continues to provide far better coverage than the health and medical press, which are almost entirely ignoring Long Covid. Simply stunning dereliction.
Meals skipped, lights shut off: Long COVID linked to severe financial strains, researchers say
https://www.marketwatch.com/story/m...re-financial-strains-researchers-say-30149eed
Paid sick leave, the social safety net, won't cut it here. It's too many people. Even if most are only ill for weeks and months, there's a never-ending mass of them, disability systems would have to be at least 4-5x as large and there's no appetite for this. Effective treatments are the only way out. I'm not even sure if we can do mitigations to prevent infections anymore, giving up early was a one-way street.
Meals skipped, lights shut off: Long COVID linked to severe financial strains, researchers say
https://www.marketwatch.com/story/m...re-financial-strains-researchers-say-30149eed
One in 10 adults with long COVID say they stopped working because of their symptoms, according to an Urban Institute study based on a survey conducted late last year. Only about six in 10 adults with long COVID reported having access to paid sick leave at work, compared with 68% of all workers, according to the study.
Over 40% of people with long COVID report having inadequate food for their household, the research shows, compared with 20% of adults who have had COVID-19 but do not have long COVID. Difficulties paying the rent or mortgage and utility bills were also far more common among people with long COVID than those without, the researchers found.
...
Lack of access to paid sick leave is driving many patients with long COVID to cut back on other activities so that they can continue working, which can also add to financial strains if people need to pay for child care or other services, researchers say. One in four people with long COVID said they had cut back on nonwork activities such as errands or chores at home so they could keep working, according to the Urban Institute report.
Over 40% of people with long COVID report having inadequate food for their household, the research shows, compared with 20% of adults who have had COVID-19 but do not have long COVID. Difficulties paying the rent or mortgage and utility bills were also far more common among people with long COVID than those without, the researchers found.
...
Lack of access to paid sick leave is driving many patients with long COVID to cut back on other activities so that they can continue working, which can also add to financial strains if people need to pay for child care or other services, researchers say. One in four people with long COVID said they had cut back on nonwork activities such as errands or chores at home so they could keep working, according to the Urban Institute report.
Paid sick leave, the social safety net, won't cut it here. It's too many people. Even if most are only ill for weeks and months, there's a never-ending mass of them, disability systems would have to be at least 4-5x as large and there's no appetite for this. Effective treatments are the only way out. I'm not even sure if we can do mitigations to prevent infections anymore, giving up early was a one-way street.
rvallee
Senior Member (Voting Rights)
The NIH has a community engagement account. A few days ago it posted a ridiculous "talk to your doctor about Long Covid for a treatment plan", and got massively criticized for spreading fiction.
And in response, their community engagement has been to hide replies. Not sure if they know that hidden replies can easily be viewed, but there it is.
Hidden replied can be viewed here. Also notable that they're admitting that even asymptomatic acute illness can lead to LC. Which destroys all the fiction around "fear" and "anxiety" and especially deconditioning after weeks of inactivity. And the CDC recently admitted that repeat infections can cause cumulative harm.
All very quietly, but we'll still hear all about it was spreading fear about it that causes Long Covid, and "lockdowns" and "immunity debt" and whatnot. What a mess this profession is.
And in response, their community engagement has been to hide replies. Not sure if they know that hidden replies can easily be viewed, but there it is.
Some people don't feel sick when they have #COVID19 but develop symptoms of #LongCOVID later on. If this sounds familiar, speak with your health care provider to find a treatment plan that works for you. Learn more about Long COVID at https://bit.ly/3ZqvDFc
Hidden replied can be viewed here. Also notable that they're admitting that even asymptomatic acute illness can lead to LC. Which destroys all the fiction around "fear" and "anxiety" and especially deconditioning after weeks of inactivity. And the CDC recently admitted that repeat infections can cause cumulative harm.
All very quietly, but we'll still hear all about it was spreading fear about it that causes Long Covid, and "lockdowns" and "immunity debt" and whatnot. What a mess this profession is.
Kalliope
Senior Member (Voting Rights)
MarketWatch Meals skipped, lights shut off: Long COVID linked to severe financial strains, researchers say
quote:
One in 10 adults with long COVID say they stopped working because of their symptoms, according to an Urban Institute study based on a survey conducted late last year. Only about six in 10 adults with long COVID reported having access to paid sick leave at work, compared with 68% of all workers, according to the study.
Over 40% of people with long COVID report having inadequate food for their household, the research shows, compared with 20% of adults who have had COVID-19 but do not have long COVID. Difficulties paying the rent or mortgage and utility bills were also far more common among people with long COVID than those without, the researchers found.
In long-COVID patient communities, it’s common to hear of “people who are losing their homes, unable to afford their next meal, having to move in with family members or friends in order to survive,” said Lisa McCorkell, a co-author of the study who is also living with long COVID.
quote:
One in 10 adults with long COVID say they stopped working because of their symptoms, according to an Urban Institute study based on a survey conducted late last year. Only about six in 10 adults with long COVID reported having access to paid sick leave at work, compared with 68% of all workers, according to the study.
Over 40% of people with long COVID report having inadequate food for their household, the research shows, compared with 20% of adults who have had COVID-19 but do not have long COVID. Difficulties paying the rent or mortgage and utility bills were also far more common among people with long COVID than those without, the researchers found.
In long-COVID patient communities, it’s common to hear of “people who are losing their homes, unable to afford their next meal, having to move in with family members or friends in order to survive,” said Lisa McCorkell, a co-author of the study who is also living with long COVID.
Art Vandelay
Senior Member (Voting Rights)
This article in some Australian Sunday newspapers covers two people with Long Covid:
Archive link in case of paywall: https://archive.li/yTU5v
Two Covid survivors speak of trauma and ongoing effects of ‘Long Covid’
Sophie van Reijswoud went from a healthy teen to vomiting 40 times a day and being tube fed. Now, her parents share the trauma and ongoing effects of “Long Covid”.
The 15-year-old got Covid in March 2022, and her parents say she has never recovered since.
She has spent nearly a year of the past 18 months in a hospital.
‘NIGHTMARE’: QLD DOCTOR’S HARROWING ORDEAL
For 16 months, Melanie Broadley has been living a nightmare.
The 32-year-old from Brisbane — who ironically is a postdoctoral researcher looking at the psychological aspects of living with a chronic illness — is among thousands of Australians quietly suffering with debilitating symptoms from long Covid.
Dr Broadley’s condition is so bad, she spends up to 20 hours a day in bed and is unable to work or go out with her husband and friends.
“I have so many symptoms. Shortness of breath, a persistent cough, extreme fatigue, heart palpitations, chest pain, sleep difficulties and sensory issues like blurred vision and ringing in the ears,” Dr Broadley said.
“Even going for a short walk around my neighbourhood is enough to trigger a crash. Along with these debilitating symptoms, I have experienced a loss of identity.
“Prior to Covid, I was an avid reader, but due to my cognitive symptoms I haven’t been able to read a single novel in over a year.”
Archive link in case of paywall: https://archive.li/yTU5v
Last edited:
rvallee
Senior Member (Voting Rights)
The NIH has a community engagement account. A few days ago it posted a ridiculous "talk to your doctor about Long Covid for a treatment plan", and got massively criticized for spreading fiction.
And in response, their community engagement has been to hide replies. Not sure if they know that hidden replies can easily be viewed, but there it is.
Hidden replied can be viewed here. Also notable that they're admitting that even asymptomatic acute illness can lead to LC. Which destroys all the fiction around "fear" and "anxiety" and especially deconditioning after weeks of inactivity. And the CDC recently admitted that repeat infections can cause cumulative harm.
All very quietly, but we'll still hear all about it was spreading fear about it that causes Long Covid, and "lockdowns" and "immunity debt" and whatnot. What a mess this profession is.
Well, the good thing is that this has blown up quite a bit. Many more replies and re-tweets have been added. It's actually emphasizing how their complete lack of urgency looks terrible. But I guess it only looks terrible if you're a patient waiting on them, so...
They don't seem to feel the need to actually say something about it. Not even a perfunctory "uh, message received, we're listening". Very poor community engagement. As in literally none whatsoever, one-way communication, and based on a blatant lie. I guess only some communities deserve to be engaged with.
Sly Saint
Senior Member (Voting Rights)
The Urgent Need for Better Support and Treatment for Long COVID
https://www.expresshealthcaremgmt.c...people-where-is-the-urgency-to-treat-it/3139/In the midst of a world that has largely moved on from pandemic safety protocols, there is a lack of urgency when it comes to treating and supporting individuals with long COVID. While significant efforts were made early on in the pandemic to prevent and treat COVID-19, the response to long COVID has been muted.
Many individuals, like Nancy Rose of Port Jefferson, N.Y., continue to suffer from long-haul symptoms, such as brain fog and memory difficulties, long after contracting COVID-19. The low quality of life experienced by millions with long COVID has seemingly been deemed acceptable in the rush to declare the pandemic over. However, this is not acceptable.
Long COVID can include a wide range of debilitating effects, including extreme fatigue, cardiac dysfunction, and memory loss. It leaves many with a quality of life worse than what people with advanced cancer experience. It is estimated that at least 65 million people worldwide and 6% of adults in the United States live with long COVID, and new cases are still being added every day.
Despite the growing number of individuals suffering from long COVID, there is a lack of support and treatment options. Clinical trials related to long COVID are underway, but most have small sample sizes and may miss more subtle effects. Some trials even use graded exercise therapy, which has been shown to worsen symptoms in a significant number of long COVID patients.
The lack of near-term treatment options leaves individuals with long COVID to resort to experimental medications or off-label drug use, which can be risky and provide mixed results. Researchers and physicians are often unwilling to prescribe treatments without robust trials supporting their effectiveness.
Congress should be incentivized to address this issue from an economic perspective. Helping individuals with long COVID improve their health and return to the workforce would boost economic productivity and reduce healthcare costs. The estimated total economic cost of long COVID was $3.7 trillion as of July 2022. Funding better clinical trials would provide patients with real answers and be significantly less expensive than letting them suffer.
Unfortunately, the lack of response to long COVID is not surprising, as chronic conditions, particularly those more common in women, have historically been neglected. For example, myalgic encephalomyelitis (ME/CFS) has been dismissed and under-researched for decades. About half of long COVID patients meet the diagnostic criteria for ME/CFS.
Mij
Senior Member (Voting Rights)
Opinion: Long Covid is debiltating to me and 65 million other people. Where is the urgency to treat it?
Without near-term treatment, those of us with long COVID are left to choose between doing nothing to alleviate our suffering and using anecdotes to make our own treatment decisions. We often resort to taking experimental medications or requesting drugs off label, which can pose safety risks and have mixed results in improving quality of life. It’s understandable why many people with long COVID want to try anything that might help, but some researchers and physicians are unwilling to prescribe treatments without robust trials supporting their effectiveness.
https://www.latimes.com/opinion/story/2023-07-31/long-covid-prevalence-research-treatments
Without near-term treatment, those of us with long COVID are left to choose between doing nothing to alleviate our suffering and using anecdotes to make our own treatment decisions. We often resort to taking experimental medications or requesting drugs off label, which can pose safety risks and have mixed results in improving quality of life. It’s understandable why many people with long COVID want to try anything that might help, but some researchers and physicians are unwilling to prescribe treatments without robust trials supporting their effectiveness.
https://www.latimes.com/opinion/story/2023-07-31/long-covid-prevalence-research-treatments
rvallee
Senior Member (Voting Rights)
Opinion: Long Covid is debiltating to me and 65 million other people. Where is the urgency to treat it?
Without near-term treatment, those of us with long COVID are left to choose between doing nothing to alleviate our suffering and using anecdotes to make our own treatment decisions. We often resort to taking experimental medications or requesting drugs off label, which can pose safety risks and have mixed results in improving quality of life. It’s understandable why many people with long COVID want to try anything that might help, but some researchers and physicians are unwilling to prescribe treatments without robust trials supporting their effectiveness.
https://www.latimes.com/opinion/story/2023-07-31/long-covid-prevalence-research-treatments
Unfortunately, our country’s (lack of) response to long COVID is not surprising, as we have a dark history of neglecting chronic conditions, particularly those that are more common in women. For example, myalgic encephalomyelitis (sometimes referred to as chronic fatigue syndrome) has been dismissed and under-researched for decades. The lack of research has perpetuated a limited understanding of the underlying biology, a lack of diagnostic testing, a lack of respect for patient experiences and an embarrassing lack of action. Research funding is extremely low relative to the burden of the disease and its prevalence.
Although this applies to every single country.
Sly Saint
Senior Member (Voting Rights)
slight variations of this seems to be doing the rounds in many publications:
Brain fog and 200 other long-term COVID symptoms focus of new study: ‘A year or two late’
eta:
"The Associated Press Health and Science Department receives support from the Howard Hughes Medical Institute’s Science and Educational Media Group. The AP is solely responsible for all content."
Brain fog and 200 other long-term COVID symptoms focus of new study: ‘A year or two late’
WASHINGTON — The National Institutes of Health is beginning a handful of studies to test possible treatments for long COVID, an anxiously awaited step in U.S. efforts against the mysterious condition that afflicts millions.
Monday’s announcement from the NIH’s $1.15 billion RECOVER project comes amid frustration from patients who’ve struggled for months or even years with sometimes-disabling health problems — with no proven treatments and only a smattering of rigorous studies to test potential ones.
“This is a year or two late and smaller in scope than one would hope but nevertheless it’s a step in the right direction,” said Dr. Ziyad Al-Aly of Washington University in St. Louis, who isn’t involved with NIH’s project but whose own research highlighted long COVID’s toll. Getting answers is critical, he added, because “there’s a lot of people out there exploiting patients’ vulnerability” with unproven therapies.
Scientists don’t yet know what causes long COVID, the catchall term for about 200 widely varying symptoms. Between 10% and 30% of people are estimated to have experienced some form of long COVID after recovering from a coronavirus infection, a risk that has dropped somewhat since early in the pandemic.
“If I get 10 people, I get 10 answers of what long COVID really is,” U.S. Health and Human Services Secretary Xavier Becerra said.
https://nypost.com/2023/07/31/200-long-term-covid-symptoms-focus-of-new-study/That’s why so far the RECOVER initiative has tracked 24,000 patients in observational studies to help define the most common and burdensome symptoms –- findings that now are shaping multipronged treatment trials. The first two will look at:
— Whether taking up to 25 days of Pfizer’s antiviral drug Paxlovid could ease long COVID, because of a theory that some live coronavirus, or its remnants, may hide in the body and trigger the disorder. Normally Paxlovid is used when people first get infected and for just five days.
— Treatments for “brain fog” and other cognitive problems. They include Posit Science Corp.’s BrainHQ cognitive training program, another called PASC-Cognitive Recovery by New York City’s Mount Sinai Health System, and a Soterix Medical device that electrically stimulates brain circuits.
Two additional studies will open in the coming months. One will test treatments for sleep problems. The other will target problems with the autonomic nervous system — which controls unconscious functions like breathing and heartbeat — including the disorder called POTS.
A more controversial study of exercise intolerance and fatigue also is planned, with NIH seeking input from some patient groups worried that exercise may do more harm than good for certain long COVID sufferers.
The trials are enrolling 300 to 900 adult participants for now but have the potential to grow. Unlike typical experiments that test one treatment at a time, these more flexible “platform studies” will let NIH add additional potential therapies on a rolling basis.
eta:
"The Associated Press Health and Science Department receives support from the Howard Hughes Medical Institute’s Science and Educational Media Group. The AP is solely responsible for all content."
rvallee
Senior Member (Voting Rights)
Janet Dafoe to Tedros Adhanom Ghebreyesus (head of WHO) said:You were said you were going to contact us. Ronald W. Davis, PHD, professor of Biochemistry & Genetics, Stanford univ, who is doing full-time research on MECFS and is a leader in the field. We never heard from you. He used to run a program at WHO. I am his wife. Offer still open!
Let's see if it can be followed through, maybe a bit of community pressure.Tedros Adhanom Ghebreyesus said:I would be happy to.
Ariel
Senior Member (Voting Rights)
EDIT: Janet Dafoe: "The director of Dr Tedros’ office just called me. Ron and I spoke with her at length. She is lovely! We were able to tell her a lot of things and Ron offered to work with WHO like he did in the past and she was just really interested in all of it. Tedros will follow up soon"
Dx Revision Watch
Senior Member (Voting Rights)
That's what Ghebreyesus said several years ago. "We hear you" and stuff about reaching out. Did he, then? No, he did not. I do not trust the WHO as far as I can spit.
rvallee
Senior Member (Voting Rights)
Worth trying again and putting some pressure, with the added "you said so last time". These things can be frustrating to make happen but once the door is open it becomes easier.That's what Ghebreyesus said several years ago. "We hear you" and stuff about reaching out. Did he, then? No, he did not. I do not trust the WHO as far as I can spit.
Wyva
Senior Member (Voting Rights)
The Boston Globe: Actually, we can’t yet ‘ignore COVID’
Responses from readers to an article written by Dr Ashish Jha and which was titled “With a few basic steps, most of us can finally ignore COVID”
There were two pop-up windows for me, I closed one and refreshed the page afterwards and the other one went away too. But I think some people couldn't access a similar article in the past though.
Responses from readers to an article written by Dr Ashish Jha and which was titled “With a few basic steps, most of us can finally ignore COVID”
There were two pop-up windows for me, I closed one and refreshed the page afterwards and the other one went away too. But I think some people couldn't access a similar article in the past though.
That's what Ghebreyesus said several years ago. "We hear you" and stuff about reaching out. Did he, then? No, he did not. I do not trust the WHO as far as I can spit.
At first glance I thought it odd that Janet would so openly discuss the talks she's having with the people at the WHO. But in this context it makes sense. Create some sort of public record of them promising things. Then if they back-track it's likely to cause at worst a bit of dissent, at best a whirlwind. I think as a community we've been poor at getting our grievances known to the public and actions like these serve us well.
Andy
Senior Member (Voting rights)
I don't think we should get our hopes up, as far as I'm aware nothing came of this, International: World Health Organization News (news relevant to ME/CFS, Long Covid and related conditions)At first glance I thought it odd that Janet would so openly discuss the talks she's having with the people at the WHO. But in this context it makes sense. Create some sort of public record of them promising things. Then if they back-track it's likely to cause at worst a bit of dissent, at best a whirlwind. I think as a community we've been poor at getting our grievances known to the public and actions like these serve us well.
I don't think we should get our hopes up, as far as I'm aware nothing came of this, International: World Health Organization News (news relevant to ME/CFS, Long Covid and related conditions)
I'm not getting my hopes up with regards to anything ME-related. I do see a slowly shifting tide and I think all the little things we and the people that care for us do, have an impact on that. Where that'll lead, I don't know.
- Status
- Not open for further replies.
