- ME/CFS is a genetically primed failure to extinguish an interferon-coupled integrated stress response after a trigger (infection or non-viral/toxic). Mitochondrial and ER damage release danger nucleic acids and misfolded proteins that activate RLR/cGAS–STING and type I/III interferons. Defects in vesicle trafficking and ER‑phagy prevent proper localization and shutdown of these pathways and of IFN receptor signaling. The result is a chronic, low‑grade IFN tone that sustains the ISR (driving elevated FGF21), shifts lipid metabolism toward phospholipid peroxidation and depletion, and propagates immune, microvascular, and neuro-autonomic dysfunction.
Why this fits the genetics (priority-coded)
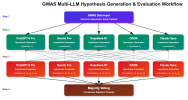
- GWAS (highest priority)
- RABGAP1L, ARFGEF2: Endosome–Golgi–plasma membrane trafficking and receptor recycling. Control STING/TLR movement and IFNAR endocytosis/recycling; impaired trafficking → prolonged or mislocalized IFN signaling and poor resolution.
- CCPG1: ER‑phagy receptor clearing stressed ER membranes that harbor STING/TLR complexes; inefficiency → sustained IFN and UPR activity.
- FBXL4: Mitochondrial DNA/biogenesis maintenance; distress releases mtDNA/RNA that drive cGAS–STING/RLR and upregulates mitokines like FGF21.
- SUDS3: SIN3/HDAC corepressor component shaping global stress/immune transcription, including ISGs; variants bias cells toward persistent “conservation” programs.
- BTN2A2: Butyrophilin co‑regulator of T and γδ T cells, tuning IFN‑γ and co‑stimulation set‑points.
- OLFM4: Neutrophil/gut crypt factor linking mucosal innate immunity and type III IFN (IFN‑λ) at barrier sites.
- CA10: Brain-enriched synaptic modulator; explains central/autonomic phenotypes in the setting of systemic IFN/ISR and vascular change.
- Tier 1 (high-confidence colocalized; highlights by pathway)
- IFN sensors/regulators: ZNFX1 (dsRNA sensing/mtRNA handling), TRIM38 (E3 ligase gating TLR/cGAS–STING amplitude/termination), RC3H1/Roquin (post‑transcriptional braking of immune mRNAs), ZBTB37/ZNF322/HMGN4 (chromatin states of ISGs).
- Trafficking/clearance: KLHL20 (Cullin3 E3; autophagy programs), CSE1L (nuclear/secretory transport), B4GALT5 (glycosphingolipid rafts affecting TLR/IFN signaling domains), STAU1 (stress granules that scaffold RLR signaling), DDX27/ABT1 (ribosome biogenesis coupling to antiviral translation control), DDX27 also impacts nucleolar stress.
- Mitochondrial/ISR: DARS2 (mt-aaRS; mitochondrial translation stress → ISR/FGF21), ZNFX1 as above.
- Lipid redox and eicosanoids: PRDX6 (peroxidase/iPLA2; repairs yet consumes phospholipids), PEBP1/RKIP (enables 15‑LOX–PE peroxidation; also modulates NF‑κB/MAPK), HFE (iron redox), PTGIS (prostacyclin synthase; endothelial tone), SERPINC1 (antithrombin; thromboinflammation).
- Immune co-stimulation/barrier: TNFSF4/OX40L, BTN3A3, VSIG10; SLC9C2 (endosomal/epithelial pH influencing TLR compartments).
- Additional: GPR52 (CNS cAMP; autonomic modulation), PEBP1 and PEBP1–15‑LOX ferroptotic signaling interface with lipid peroxidation.
- Tier 2 (nearest-gene where Tier 1 was absent): FBXL4, OLFM4, CCPG1 (also GWAS hits) reinforce the mitochondrial, mucosal, and ER‑phagy axes.
Mechanistic chain (now explicit for IFN)
1) Trigger (virus, bacterial products, organophosphates/toxins, ischemic stress) perturbs membranes, Ca2+, and redox → ER misfolding and mitochondrial ROS/damage.
2) Mito‑nucleic acid release activates RLRs and cGAS–STING → type I IFN (α/β); mucosal sites emphasize type III IFN (λ). T/NK circuits contribute type II IFN (γ) depending on BTN/OX40L set‑points.
3) Trafficking and ER‑phagy resolution fails: ARFGEF2/RABGAP1L mis-handle STING/TLR/IFNAR trafficking; CCPG1‑dependent ER‑phagy clears poorly. TRIM38/RC3H1/ZNFX1/ STAU1/DDX27 set abnormal on/off kinetics. Net effect: tonic, spatially mislocalized IFN signaling.
4) IFN–ISR coupling: dsRNA‑PKR and PERK phosphorylate eIF2α; translation throttles, ATF4/CHOP programs engage, and FGF21 rises as a systemic mitokine.
5) Lipid injury and depletion: PRDX6 and PEBP1–15‑LOX drive phospholipid peroxidation and lyso‑PL generation; HFE‑linked iron accelerates lipid ROS. B4GALT5‑dependent raft changes alter TLR/IFN microdomains. Plasma phosphatidylcholines/PE fall, oxidized/lyso‑PLs rise.
6) Vascular/coagulation: PTGIS and SERPINC1 axes shift toward endothelial dysfunction, platelet activation, and microclots, impairing oxygen delivery and recovery after exertion.
7) Immune set‑point: BTN2A2/BTN3A3 and TNFSF4/OX40L reshape T and γδ T‑cell circuits in a background of tonic IFN, favoring poorly resolving inflammation and post‑exertional exacerbations.
8) CNS/autonomic: CA10/GPR52 plus systemic IFN/ISR and microvascular change yield cognitive, sensory, and orthostatic symptoms.
Why non‑viral triggers fit
- Toxins such as organophosphates can cause mitochondrial/ER damage and lipid peroxidation, releasing DAMPs (mtDNA/RNA) that drive cGAS–STING/RLR and IFN without infection. The shared bottleneck is resolution capacity (trafficking + ER‑phagy), not the trigger’s origin.
Key predictions (falsifiable)
- Whole blood or single-cell ISG signatures show tonic elevation with altered kinetics (prolonged TBK1/IRF3–STAT1/2 signaling, blunted receptor recycling).
- Patient cells display delayed STING trafficking to lysosomes and impaired shutdown; defects correlate with ARFGEF2/RABGAP1L alleles; CCPG1 loss-of-function phenotypes show reduced ER‑phagy flux.
- Post‑exertion, transient spikes in cell‑free mtDNA and type I/III IFNs accompany rises in FGF21 and lipid peroxidation adducts (e.g., 4‑HNE; 15‑LOX–PE species).
- Plasma lipidomics: reduced PCs/PEs, elevated lyso‑PLs/oxidized‑PLs; altered glycosphingolipids (B4GALT5).
- Endothelial tests: lower prostacyclin metabolites, antithrombin imbalance, increased thromboinflammatory/microclot markers.
- Gut-dominant phenotypes show stronger IFN‑λ signatures and OLFM4‑linked neutrophil/NET activity.
Implications (research directions, not clinical advice)
- Restore resolution of IFN signaling: target STING/TLR trafficking and degradation (autophagy/lysosomal enhancers; carefully titrated STING modulators); bolster CCPG1‑axis ER‑phagy.
- Tune the ISR rather than blanket immunosuppression: timed ISR modulators; support mitochondrial translation/biogenesis in genetically susceptible backgrounds (e.g., FBXL4/DARS2 contexts).
- Repair membrane composition and limit ferroptotic chemistry: plasmalogen/phospholipid repletion, inhibitors of PEBP1–15‑LOX complexes, iron handling support; antioxidant strategies targeted to membranes.
- Improve microvascular tone/antithrombotic balance: prostacyclin pathway, antithrombin support, careful platelet modulation.
- Calibrate costimulatory axes: BTN/OX40L pathway research to reset T/γδ T‑cell set‑points without ablating host defense.
In short: ME/CFS may be a “failure to extinguish IFN‑coupled stress” disorder. Genetic variation in trafficking (RABGAP1L, ARFGEF2), ER‑phagy (CCPG1), mitochondrial maintenance/translation (FBXL4, DARS2), transcriptional control (SUDS3), and immune set‑points (BTN2A2 and others) biases recovery toward a chronic state with tonic IFN, sustained ISR (FGF21‑high), and phospholipid injury (phospholipids‑low), producing the multi‑system phenotype.