As some of you are already aware, I am leaving this forum in the next day or so.
Before I go, I'd like to drop the following here, in relation to this 2020 EURONET-SOMA paper and related issues.
A PDF copy of an earlier paper published on behalf of the EURONET-SOMA Group can be downloaded, here:
https://umu.diva-portal.org/smash/get/diva2:1211391/FULLTEXT01.pdf
I was amused to see that my 2017 submission for the deletion of the BDD category from ICD-11 is referenced in this earlier paper (at Ref 26).
This is what Fink said in relation to his terrible disappointed with the WHO and ICD-11, in an article published by his cronies following his lecture on the occasion of his 2017 Alison Creed Award:
Note that where Fink writes:
"To include the BDS/BSD diagnosis and all relevant functional somatic syndromes..."
he should have said
/BSS (which is the proposal of the Goldberg led PCCG advisory group for the development of the WHO's ICD-11 PHC).
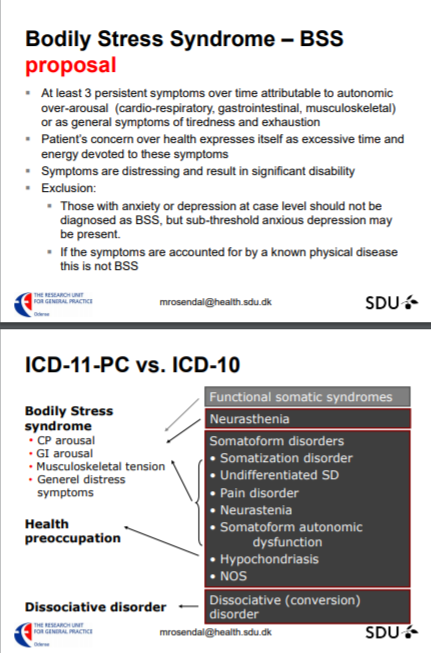
The PCCG group's proposed construct had originally been referred to by the group's chair as "Bodily distress syndrome" (same as Fink's term) and their proposed disorder construct and criteria had been adapted from Fink's BDS - so it was not a "pure" BDS criteria set or disorder description.
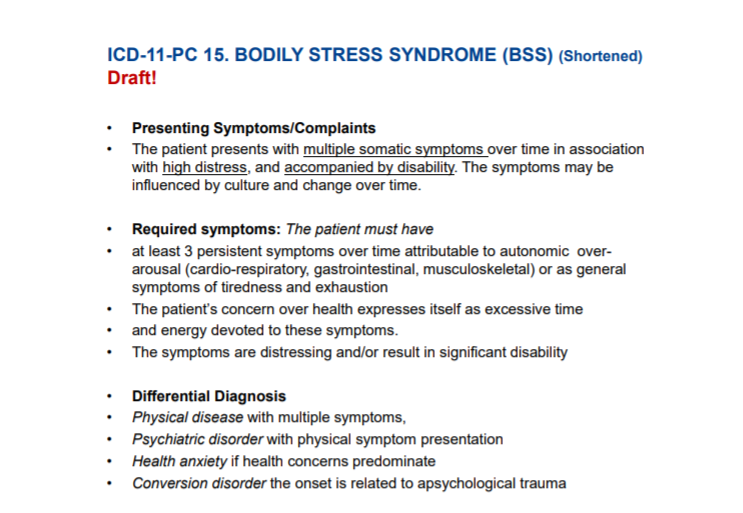
Later, they revised the proposed name to "Bodily Stress Syndrome (
BSS)" and modified their proposed criteria to:
"This proposes a specific number of symptoms not otherwise explained and largely related to a postulated underlying mechanism of autonomic arousal"
The presentation slides that accompanied Fink's Alison Creed Award lecture are archived on my site here:
https://dxrevisionwatch.files.wordpress.com/2019/09/plenary_prof_fink.pdf
In those slides, is a brief summary of the essential features for the ICD-11 PHC's proposed
revised criteria:
See also:
MUS becomes Bodily Stress Syndrome in the ICD-11 for primary care Results from the WHO Primary Care Consultation Group on mental health Marianne Rosendal
https://dxrevisionwatch.files.wordp...are-consultation-group-on-mental-health-1.pdf
ICD-11 PHC (aka ICD-11 PC, ICD-11-PHC):
The WHO's ICD-11 PHC is a clinical guideline written in simpler language to assist non-mental health specialists with the diagnosis and management of common mental disorders (especially primary care practitioners and non medically trained health workers, and is also intended for use in low resource settings and in low- to middle-income countries).
The ICD-11 PHC is still under development and is a revision of the
Diagnostic and Management Guidelines for Mental Disorders in Primary Care: ICD-10 Chapter V Primary Care Version. 1996. Copy archived on WHO's IRIS site here:
https://apps.who.int/iris/handle/10665/41852.
The committee that developed the 1996 edition had been chaired by Prof Sir David Goldberg and Goldberg, now is his mid 80s, is also chairing the advisory group making recommendations to the WHO for the revised edition.
The ICD-11 PHC is proposed to comprise just 27 "common mental disorders"
and it contains no general medical disorders or diseases.
Like the ICD-10 PHC (1996) edition, this revised diagnostic and management guideline
will not be a mandatory classification for WHO Member States - although the WHO hopes the new version will have greater utility and uptake than the 1996 version had.
For
the mandatory core ICD-11 classification, as we know, the WHO is going forward with the SSD-like Bodily distress disorder (BDD).
But the ICD-11 PHC is proposed to include a differently conceptualised disorder category called "Bodily Stress Syndrome (BSS)" with different criteria.
So the construct already approved for the mandatory core ICD-11 does not align with the construct being proposed for the primary care 27 mental disorder guideline.
The full draft texts for the 27 mental disorder categories proposed for inclusion in the ICD-11 PHC have not been made available for public scrutiny, but a number of progress papers, field trial evaluations and presentations have been published since 2010.
So we can rely only on the progress papers, on the Protocol document for the field trials, and on presentations [1][2][3][4].
In field trial evaluation paper [1], under exclusions and differential diagnoses for BSS, certain psychiatric, and general medical diagnoses have to be excluded but CFS, ME; IBS; and FM appear not to be specified as exclusions.
(As you know, I have recently obtained exclusions for PVFS; BME; and CFS under the core ICD-11's Bodily distress disorder.)
When it has been finalised and released, the WHO has said it intends to make the ICD-11 PHC available on its website for free download. It's not known when this guideline is expected to be made available. The core ICD-11 edition's companion publication for psychiatrists (the CDDG for Mental and behavioural disorders) has not been finalised or released yet, either.
ICPC-2:
Note that for primary care, some EU countries have a long history of use of the WONCA developed and WHO endorsed,
International Classification of Primary Care (ICPC-2). This includes abridged categories for mental and behavioural disorders and general medical conditions and diseases plus other terminology used in general practice settings.
ICPC-2 is available in 34 countries; is used in primary care in 27 countries and is mandatory in 6 EU countries, eg the Netherlands.
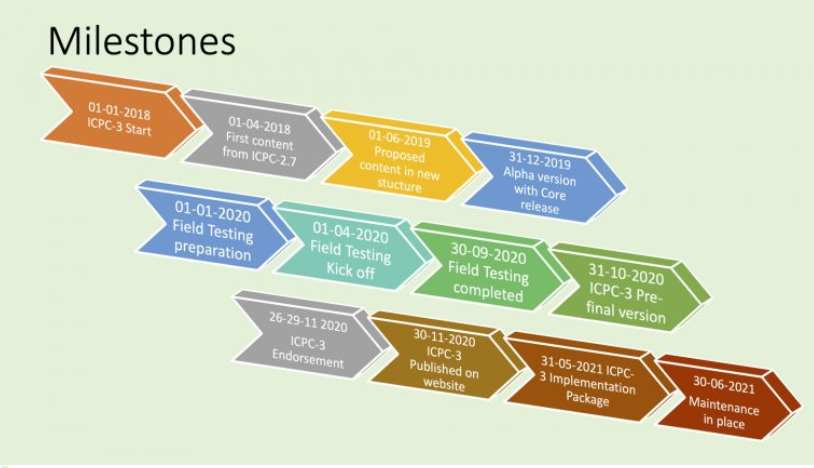
ICPC-2 is currently under revision for
ICPC-3.
The content of ICPC-3 is intended to be linked to relevant classifications, such as ICD-10, ICD-11, ICF, ICHI, DSM-5, to clinical terminologies such as SNOMED-CT, but also to previous versions of ICPC.
The draft content for ICPC-3 is not being developed on a publicly accessible platform and it's unclear whether any form of stakeholder review will be undertaken, or at what point.
Dr Marianne Rosendal (Aarhus University), who has published with Prof Per Fink, is the European representative on WONCA's International Classification Committee and a member of the revision committee for ICPC-2, as is the U.S.'s, Dr Michael Klinkman. Both of these have been members of the ICD-11 PHC PCCG advisory group, with Klinkman acting as the PCCG group's Vice-chair.
ICPC-2 meeting summary documents dating from 2010/2011, that I have on file, indicate that Rosendal had discussed the potential for a Bodily distress syndrome or a similar disorder concept for inclusion in the ICPC-3. Per Fink is likely to have been lobbying hard for its inclusion, especially as he failed in his bid to get BDS into the core ICD-11.
The development of ICPC-3 will need very close monitoring. It's due to be finalised later this year, but I suspect the current projected timeline will need to be extended:
References:
1 T P Lam, D P Goldberg, A C Dowell, S Fortes, J K Mbatia, F A Minhas, M S Klinkman. Proposed new diagnoses of anxious depression and bodily stress syndrome in ICD-11-PHC: an international focus group study,
Family Practice, Volume 30, Issue 1, February 2013, Pages 76–87,
https://doi.org/10.1093/fampra/cms037
2 MASTER PROTOCOL Depression, Anxiety and Somatic Symptoms in Global Primary Care Settings: A Field Study for the ICD-11-PHC Version 2 for WHO Research Ethics Review Committee.
https://dxrevisionwatch.files.wordpress.com/2020/03/master-protocol_icd_11_phc_field_study_2.pdf
3 Fortes, Sandra, Ziebold, Carolina, Reed, Geoffrey M, Robles-Garcia, Rebeca, Campos, Monica R, Reisdorfer, Emilene, Prado, Ricardo, Goldberg, David, Gask, Linda, & Mari, Jair J.. (2019). Studying ICD-11 Primary Health Care bodily stress syndrome in Brazil: do many functional disorders represent just one syndrome?
Brazilian Journal of Psychiatry, 41(1), 15-21. Epub October 11, 2018.
Html:
https://dx.doi.org/10.1590/1516-4446-2018-0003
PDF:
http://www.scielo.br/pdf/rbp/v41n1/1516-4446-rbp-1516444620180003.pdf
4 Presentation: Rosendale, M (2017).
MUS becomes Bodily Stress Syndrome in the ICD-11 for primary care
--------------------------------
So that's it from me, folks.
If I need to post an update on the status of the IAPT lead's November submission for adding DSM-5's Somatic symptom disorder (SSD) into the UK Edition of SNOMED CT, in order to obtain the SSD term and a SNOMED CT Concept code/ICD-10 map code for use in its new IAPT Data Set v2.0, due to implement from April 01;
or if there is a development with my new proposal [5] for removing the "Benign" prefix from "Benign myalgic encephalomyeltis" for ICD-11, one of the moderators has very kindly offered to post a statement on my behalf.
5 Proposal for removing "Benign" prefix from "Benign myalgic encephalomyeltis" for ICD-11, Suzy Chapman, submitted February 14, 2020:
https://dxrevisionwatch.files.wordpress.com/2020/02/new-proposal-for-icd-11-remove-benign-1.pdf
Suzy Chapman,
Dx Revision Watch
http://dxrevisionwatch.com
http://twitter.com/dxrevisionwatch
----------------------
[Edited to insert graphic for projected timeline for development of ICPC-3.]
Edit: Link in reference 2 replaced.