John Mac
Senior Member (Voting Rights)
Abstract:
Myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) is a disabling disease
with worldwide prevalence and limited therapies exclusively aimed at treating symptoms.
To gain insights into the molecular disruptions in ME/CFS, we utilized an aptamer-based technology that quantified 4790 unique human proteins, allowing us to obtain the largest proteomics dataset yet available for this disease, detecting highly abundant proteins as well as rare proteins over a ninelog dynamic range.
We report a pilot study of 20 ME/CFS patients and 20 controls, all females.
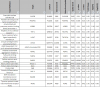
Significant differences in the levels of 19 proteins between cohorts implicate pathways related to the extracellular matrix, the immune system and cell–cell communication.
Outputs of pathway and cluster analyses robustly highlight the ephrin pathway, which is involved in cell–cell signaling and regulation of an expansive variety of biological processes, including axon guidance, angiogenesis, epithelial cell migration, and immune response.
Receiver Operating Characteristic (ROC) curve analyses distinguish the plasma proteomes of ME/CFS patients from controls with a high degree of accuracy (Area Under the Curve (AUC) > 0.85), and even higher when using protein ratios (AUC up to 0.95), that include some protein pairs with established biological relevance.
Our results illustrate the promise of plasma proteomics for diagnosing and deciphering the molecular basis of ME/CFS
https://www.mdpi.com/2227-7382/9/1/6