Grigor
Senior Member (Voting Rights)
Yes, but that's from 2018. She mentioned it maybe last year the year before.She says not in this article.
Yes, but that's from 2018. She mentioned it maybe last year the year before.She says not in this article.
My point was that at the time they had their surgery, neither had JHS, hEDS or EDS or met the criteria such as Beignton.Yes, but that's from 2018. She mentioned it maybe last year the year before.
Ah I understand. Yes, true.My point was that at the time they had their surgery, neither had JHS, hEDS or EDS or met the criteria such as Beignton.
What is JHS?My point was that at the time they had their surgery, neither had JHS, hEDS or EDS or met the criteria such as Beignton.
Joint hypermobility syndrome - which is supposed to include general pain.What is JHS?
Says this:She says not in this article.
While I am going to see an EDS geneticist after my surgery, based on symptom descriptions, I’m pretty sure I don’t meet the diagnostic criteria for classical EDS or any of the other testable forms.
As for hypermobile EDS (hEDS), the one type without a known genetic marker, I also don’t meet the current diagnostic criteria.
It would be fancy if they sell it as *the* cause of ME/CFS as Jeff Wood does. But such pressure could put the brain immune system on the edge similar to what concussion does, and we already know concussion can cause debilitating fatigue. Again, it may not be worth looking into if it's only one case (or even two). But it may be if there are several independent cases.As to conjuring up fancy mechanisms isn't a surgeon looking for custom, and dreaming up brain stem compression to sell, pretty much that?
In general, the purpose of this forum is to examine the evidence. I don’t think anyone should be expected to take anyone’s word for something.I take Rowe et al.'s report seriously because:
-- Dr. Rowe has been treating ME/CFS patients for 30 years. He therefore understands PEM and is unlikely to have misdiagnosed three patients.
I disagree.-- Dr. Rowe does not have a conflict of interest.
Hello! In support of their argument, the authors of this preprint cite a 2018 paper by Dr. Peter Rowe and colleagues.
Yes, and these two stories, one published on Wood's personal website and the other on Cort Johnson's HealthRising blog are described as "perhaps the most compelling evidence that at least a subset of ME/CFS cases are directly caused by brainstem deformation." That's concerning.From the preprint, the evidence of recovery after surgery seems to be two case studies - Jeff Wood and Jen Brea.
But, a lot more people with ME/CFS than these two have undergone neck surgery in the hope of improvement.
@Trish, I am in complete agreement. I remember when this all began, s4me members called for data to be published by the surgeons so that it could be seen what kinds of diagnoses these patients had and what the outcomes of the surgeries were, and proponents of the 'mechanical basis' theory also indicated that data would be forthcoming. If, 6 years later, they are no farther along in that pursuit, we have gone nowhere with this theory. I wish it could be put to rest.I haven't read the article, but if that's all they can come up with as recovery evidence 6 years on from Jen and Jeff doing their big social media push and setting up private facebook groups to promote the surgery, and Jeff running his business promoting it, then all this article is is advertising based on nothing.
Any prospective New Patient should contact Mr. Jeffrey Wood
(Director of Data Collection and Screening).
Email: jeffrey.wood@mountsinai.org
As a first step, Mr. Wood will collect demographic, insurance, and clinical information.
Reading their stories, it's quite obvious that Jen Brea & Jeff Wood (esp. Jen) did not have the same disorder as most people with ME/CFS. Any ME/CFS knowledgeable doctor worth their salt should have also picked up on this if they watched Unrest; literally within the first 10 min of Unrest Jen is shown having facial hemisensory loss, dystonia of the hand, and verbal apraxia while trying to say "wow." She also discussed in her TED Talk how she had difficulty drawing complete circles (indicative of visual neglect). These are not symptoms of ME/CFS!Yes, and these two stories, one published on Wood's personal website and the other on Cort Johnson's HealthRising blog are described as "perhaps the most compelling evidence that at least a subset of ME/CFS cases are directly caused by brainstem deformation." That's concerning.
Reading their stories, it's quite obvious that Jen Brea & Jeff Wood (esp. Jen) did not have the same disorder as most people with ME/CFS. Any ME/CFS knowledgeable doctor worth their salt should have also picked up on this if they watched Unrest; literally within the first 10 min of Unrest Jen is shown having facial hemisensory loss, dystonia of the hand, and verbal apraxia while trying to say "wow." She also discussed in her TED Talk how she had difficulty drawing complete circles (indicative of visual neglect). These are not symptoms of ME/CFS!
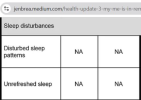
View attachment 27465
Jen also never had unrefreshing sleep or other sleep disturbances like insomnia/circadian rhythm dysfunction and therefore would not have met IOM criteria. She met ICC criteria; and CCC criteria because sleep dysfunction is not required if the illness began with an infection, which hers did. Jeff did have unrefreshing sleep, but he had sleep apnea caused by the CCI. Both Jen and Jeff both eventually developed central apnea while they were awake. They also both developed a "bobble head"/sinking head feeling. At least in Jeff's cases, his illness seemed to start as a more typical ME/CFS type presentation before these additional atypical symptoms emerged though.
Both Jen and Jeff had PEM which they both reported being quickly cured of after CCI surgery (Jeff also reported being quickly cured of PEM when he was put in a halo brace), which (if you accept anecdotes as evidence) suggests that PEM is not unique to one disorder, but if PEM is a symptom of some cases of CCI, it may have different features vs. PEM in ME/CFS. For ex, Jen reported that she never experienced a feeling of being wired or running on adrenaline, and "tired but wired" seems like an almost universal feature of PEM in ME/CFS.
She met ICC criteria; and CCC criteria because sleep dysfunction is not required if the illness began with an infection, which hers did.
