Effectiveness of Exercise-Based Rehabilitation in Chronic Fatigue Syndrome: A Systematic Review and Meta-analysis
Antonio De Vera Martín, Alberto Díaz Salazar, Isidro Miguel Martín Pérez, Sebastián Eustaquio Martín Pérez
[Line breaks added]
Abstract
Chronic Fatigue Syndrome is a complex and debilitating disorder characterized by persistent fatigue, musculoskeletal pain, sleep disturbances, and cognitive impairments. The global prevalence is estimated between 0.2% and 0.4%, affecting over 17 million individuals worldwide, with an estimated burden exceeding 40,000 cases in Spain.
Despite the exploration of exercise-based rehabilitation as a therapeutic strategy, its clinical efficacy remains a subject of ongoing debate. This study aims to evaluate the effectiveness of exercise-based rehabilitation relative to conventional treatments in improving functional capacity and alleviating fatigue among adults with CFS
A systematic review and meta-analysis were conducted following PRISMA guidelines and registered in the PROSPERO database (CRD42024573955). Searches were systematically performed across MEDLINE, PEDro, CINAHL, Google Scholar, Scopus, and SportDiscus, covering studies published between January 2010 and January 2024. Methodological quality and risk of bias, assessed using the validated PEDro Scale and Cochrane tool, ranged from moderate to good, with bias levels varying from low to high. Inclusion criteria targeted studies investigating structured therapeutic exercise interventions, including aerobic training, resistance exercises, and mind-body therapies.
A total of 11 studies were included in the qualitative review, and with 7 randomized controlled trials (n = 2,276 participants) were finally incorporated in the meta-analysis.
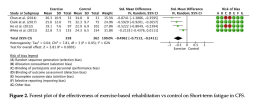
Exercise-based interventions, including aerobic training, resistance exercises, graded exercise therapy (GET), mind-body therapies and multimodal programs, showed significantly significant reductions in fatigue in both the short term (n = 720) SMD = −0.50; 95% CI: [−0.75, -0.24]; Z = 3.81; p < 0.001) and medium term (n = 501; SMD = −0.53; 95% CI: [−0.95, -0.12]; Z = 2.52; p = 0.01).
Medium-term improvements in functionality were also significant (n = 685; SMD = 0.31; 95% CI: [0.11, 0.52]; Z = 2.96; p = 0.003), whereas short-term functionality outcomes were lesser compared to controls (n = 366; SMD = 0.10; 95% CI: [−0.05, 0.25]; Z = 1.29; p = 0.20).
Notably, the meta- analytic findings indicated that medium-term functional outcomes slightly favored control groups over exercise interventions, and no significant long-term benefits were observed in either fatigue reduction or functional capacity enhancement.
These findings underscore the selective efficacy of exercise-based rehabilitation for CFS, particularly in mitigating fatigue over the short to medium term. However, the transient nature of functional improvements highlights the need for further research to optimize exercise protocols, determine the most effective modalities, and develop strategies to sustain long-term therapeutic outcomes.
While the results support exercise as a potential adjunctive therapy for CFS, they also emphasize the necessity of rigorous, longitudinal investigations to establish its clinical applicability and long-term efficacy.
Link | PDF (International Journal of Exercise Science) [Open Access]
Antonio De Vera Martín, Alberto Díaz Salazar, Isidro Miguel Martín Pérez, Sebastián Eustaquio Martín Pérez
[Line breaks added]
Abstract
Chronic Fatigue Syndrome is a complex and debilitating disorder characterized by persistent fatigue, musculoskeletal pain, sleep disturbances, and cognitive impairments. The global prevalence is estimated between 0.2% and 0.4%, affecting over 17 million individuals worldwide, with an estimated burden exceeding 40,000 cases in Spain.
Despite the exploration of exercise-based rehabilitation as a therapeutic strategy, its clinical efficacy remains a subject of ongoing debate. This study aims to evaluate the effectiveness of exercise-based rehabilitation relative to conventional treatments in improving functional capacity and alleviating fatigue among adults with CFS
A systematic review and meta-analysis were conducted following PRISMA guidelines and registered in the PROSPERO database (CRD42024573955). Searches were systematically performed across MEDLINE, PEDro, CINAHL, Google Scholar, Scopus, and SportDiscus, covering studies published between January 2010 and January 2024. Methodological quality and risk of bias, assessed using the validated PEDro Scale and Cochrane tool, ranged from moderate to good, with bias levels varying from low to high. Inclusion criteria targeted studies investigating structured therapeutic exercise interventions, including aerobic training, resistance exercises, and mind-body therapies.
A total of 11 studies were included in the qualitative review, and with 7 randomized controlled trials (n = 2,276 participants) were finally incorporated in the meta-analysis.
Exercise-based interventions, including aerobic training, resistance exercises, graded exercise therapy (GET), mind-body therapies and multimodal programs, showed significantly significant reductions in fatigue in both the short term (n = 720) SMD = −0.50; 95% CI: [−0.75, -0.24]; Z = 3.81; p < 0.001) and medium term (n = 501; SMD = −0.53; 95% CI: [−0.95, -0.12]; Z = 2.52; p = 0.01).
Medium-term improvements in functionality were also significant (n = 685; SMD = 0.31; 95% CI: [0.11, 0.52]; Z = 2.96; p = 0.003), whereas short-term functionality outcomes were lesser compared to controls (n = 366; SMD = 0.10; 95% CI: [−0.05, 0.25]; Z = 1.29; p = 0.20).
Notably, the meta- analytic findings indicated that medium-term functional outcomes slightly favored control groups over exercise interventions, and no significant long-term benefits were observed in either fatigue reduction or functional capacity enhancement.
These findings underscore the selective efficacy of exercise-based rehabilitation for CFS, particularly in mitigating fatigue over the short to medium term. However, the transient nature of functional improvements highlights the need for further research to optimize exercise protocols, determine the most effective modalities, and develop strategies to sustain long-term therapeutic outcomes.
While the results support exercise as a potential adjunctive therapy for CFS, they also emphasize the necessity of rigorous, longitudinal investigations to establish its clinical applicability and long-term efficacy.
Link | PDF (International Journal of Exercise Science) [Open Access]