You are using an out of date browser. It may not display this or other websites correctly.
You should upgrade or use an alternative browser.
You should upgrade or use an alternative browser.
Dr Karl Morten - UK researcher based at Oxford University
- Thread starter Adrian
- Start date
wigglethemouse
Senior Member (Voting Rights)
The Raman Spectroscopy work looks really interesting. From Website:
Raman Microscopy
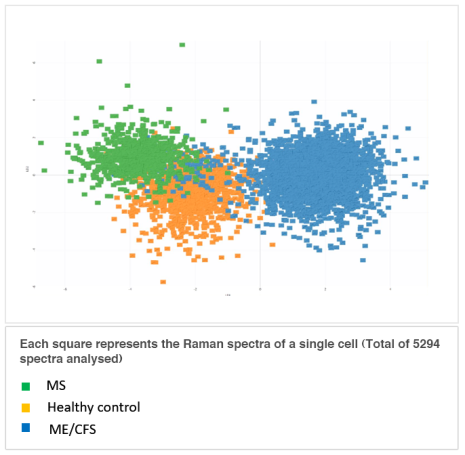
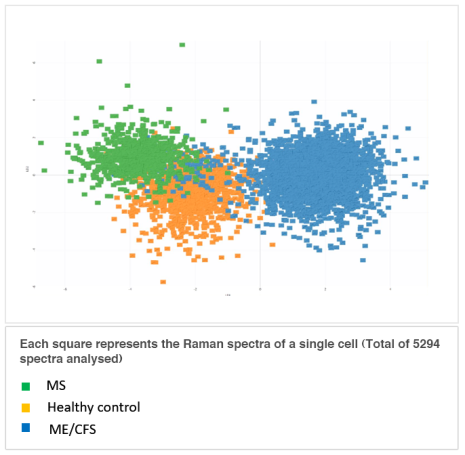
Summary of results so far (February 2019): Building on our initial data suggesting Raman microscopy of PBMC had potential as a diagnostic test in ME/CFS (Xu et al., 2019) we have looked at a further 41 subjects with ME/CFS (mild, moderate and severe), healthy controls and Multiple Sclerosis patients from the UK Biobank cohort. Our preliminary results using a combination of machine learning analysis of PBMC Raman spectra and the Zegami platform for data visualisation showed an extremely exciting separation of the 3 groups (see below), suggesting something is very different between the cells in the 3 groups.
Validation trial of our preliminary results
We now plan to continue this work by looking at a further 200 PBMC samples we have available in Oxford.
Raman Microscopy
Summary of results so far (February 2019): Building on our initial data suggesting Raman microscopy of PBMC had potential as a diagnostic test in ME/CFS (Xu et al., 2019) we have looked at a further 41 subjects with ME/CFS (mild, moderate and severe), healthy controls and Multiple Sclerosis patients from the UK Biobank cohort. Our preliminary results using a combination of machine learning analysis of PBMC Raman spectra and the Zegami platform for data visualisation showed an extremely exciting separation of the 3 groups (see below), suggesting something is very different between the cells in the 3 groups.
Validation trial of our preliminary results
We now plan to continue this work by looking at a further 200 PBMC samples we have available in Oxford.
Dolphin
Senior Member (Voting Rights)
I'm not sure when the video is from, but the video recording can be watched on their Facebook page:just went to this link and an audio started but no visual.
It's apparently a BBC South today report, but from when/where?
very odd.
ETA: The TV clip is from July 2018
Last edited:
Dolphin
Senior Member (Voting Rights)
A couple of posts today from the ME Association Facebook page
Karl Morten
Dear Kathryn The study started in 2013 when we were trying to work out if GET had any impact in this illness. At the time GET was the standard treatment offered to patients in the UK. The protocol is very different from the Pace trial with much more support in place to help patients who were struggling. The Polish group have had zero funding which is why the study has taken so long. This study is producing some very useful data around the impact of GET on a patients biology which will provide key insights into what is going on. Data is available on people who completed the 6 month programme, did not start or dropped out (The last 2 groups cover over 50% of the ME/CFS patients in the study). We have a metabolomics plasma profile on all three groups at baseline and on the GET completors when they finished the programme. Three important papers are in preparation on this cohort really digging into the impact of GET on clinical tests and biology. We need to understand why patients respond so differently to an intervention that works so well in many other conditions. This could be a major clue as to what is causing ME/CFS. ME/CFS is a looking like a heterogeneous condition and studies like this will prove really helpful. We are really not suggesting ME/CFS patients should be offered GET and are just publishing our findings. Publishing all results is really important if we are to move forwards in this illness.
Karl Morten Thank you Kathryn. We are actually starting to understand how exercise interacts with mitochondria in tissues outside muscle. See https://www.ahajournals.org/doi/10.1161/CIRCRESAHA.117.310725 . The work by Dr Bhupesh Prusty is interesting and you could imagine if mitochondria are already in a fragmented state due to ME/CFS increasing this with exercise might not be a good idea. The heart study was quite a surprise as we had always felt fragmentation of mitochondria was a bad thing. Oxford Brookes are doing some nice work on healthy subjects and Parkinson's patients exploring how exercise improves function. Great news that Helen Dawes and her team recently received funding from the MEA. I really believe things are moving forwards in ME/CFS. In the UK the most important thing is to get more clinicians interested in the condition as a research area. This is our main route into recruiting patients for clinical studies. If we can build up a UK ME/CFS research base with proper funding they will come, even if we have to import them!
Sly Saint
Senior Member (Voting Rights)
ZEGAMI JOINS TEAM OF MEDICAL RESEARCHERS TO HELP FIND THE CAUSE OF ME/CHRONIC FATIGUE SYNDROME AND ULTIMATELY A CURE
https://www.pharmiweb.com/pwtoday-s...hronic-fatigue-syndrome-and-ultimately-a-cureZegami, the Oxford University data visualisation spin-out, has joined an international team of medical researchers to try and find the cause of Myalgic Encephalomyelitis (ME) or Chronic Fatigue Syndrome (CFS). This could then help in the development of the first ever medical test for the condition, new treatments or even to find a cure. The work could also help researchers studying other medical conditions that have a fatigue symptom including cancer, strokes, Parkinson Disease and Multiple Sclerosis.
ME/CFS affects 20 million people worldwide, but it is not clear what causes it. Complex and variable symptoms make it difficult to diagnose and only 5% of patients make a full recovery. Research into the causes has been limited due to a lack of funding, but the recent identification of high levels of L-form bacteria in the blood of patients suggests they may play a role in condition.
The new research project will be the largest of its kind in Europe, involving three ME/CFS research centres (Oxford, Bydgoszcz (Poland), and Valencia) over a four to five-year period. The team, led by Dr Karl Morten from the Department of Womens and Reproductive Health, University of Oxford, has secured funding worth $750,000 from SoftCell Biologicals, who have developed a patent-pending protocol to culture and examine hidden bacteria in the circulatory system, and is looking to raise an additional £1.6 million.
The study will generate thousands of items of data, and Zegami will work with the project team to build a model using artificial intelligence and data visualisation tools to help analyse these, and more easily identify trends and patterns.. The project uses Peripheral Blood Mononuclear Cell (PBMC) data obtained from the UK ME/CFS biobank, which includes samples of ME/CFS, Multiple Sclerosis and healthy control groups. Raman spectroscopy is then used and visualised in Zegami, which was able to clearly differentiate between the three different groups. These exciting results represent an important first step in developing a diagnostic test for the bacteria. This builds on a smaller Oxford study led by Professor Wei Huang from the Department of Engineering Science (https://pubs.rsc.org/en/content/articlelanding/2019/an/c8an01437j)
The bio-resources collected during this project will be appropriately stored and made available to future studies, encouraging new investigators and clinicians into the fatigue research area. This is vital to help develop ME/CFS and fatigue as a clinical research area.
Dr Karl Morten Director of Graduate Studies and Principle Investigator, The University of Oxford said: “We hope to embark on a hugely important project to try and find out what causes ME, a question that has baffled the medical profession. Our hope is that if we can find out what causes this debilitating disease and a test can then quickly be developed to help identify when people are suffering from it. With diagnosis in many cases taking over 10 years, early detection could potentially enable patients to take steps to prevent the condition from getting worse and increasing the chances of a full recovery. The ultimate prize would be that our work would contribute to the medical profession finding new treatments and ultimately a cure.”
Andy
Senior Member (Voting rights)
https://www.epmmagazine.com/news/global-research-team-aims-to-find-cause-of-chronic-fatigue-s/Data visualisation company Zegami is collaborating with an international team of medical researchers to try and find what causes Chronic Fatigue Syndrome (CFS).
The condition, also known as Myalgic Encephalomyelitis (ME) affects around 20 million people worldwide, but it is currently not clear what causes it. A range of complex symptoms make the condition difficult to diagnose and only 5% of patients make a full recovery.
The new project involving Zegami will be the largest of its kind in Europe, including three research centres in Oxford Bydgoszcz (Poland), and Valencia, over a four to five-year period. The team has secured $750,000 in funding from SoftCell Biologicals and is looking to raise an additional £1.6 million.
SoftCell Biologicals has recently developed a patent-pending protocol to culture and examine hidden bacteria in the circulatory system. Recent research into the cause of CFS/ME has been focused on the high levels of L-form bacteria found in patients’ blood, which suggests they may play a role in the condition.
The project will use Peripheral Blood Mononuclear Cell (PBMC) data obtained from the UK ME/CFS biobank, which includes samples of ME/CFS, Multiple Sclerosis and healthy control groups. Raman spectroscopy will then be used and visualised using Zegami’s software in order to differentiate between the three groups, and also identify trends and patterns.
It’s hoped that the project will help develop the first ever medical diagnostic test for ME/CFS and could even lead to new treatments or a cure.
Andy
Senior Member (Voting rights)
Official page also up on the Nuffield Department of Women’s & Reproductive Health (part of the University of Oxford) website, https://www.wrh.ox.ac.uk/research/myalgic-encephalomyeltis-chronic-fatigue-syndrome
Andy
Senior Member (Voting rights)
"EXCITING NEW RESEARCH INITIATIVE IN ME/CFS, CHRONIC LYME DISEASE AND LONG COVID
Action for ME have agreed to fund a new PhD student project exploring the role of the leaky gut, markers of infection and the presence of pathogenic organisms in patients with ME/CFS, Chronic Lyme Disease and Long Covid.
The project is due to start in October 2021 and will look to recruit patients in 2022.
Action for ME have agreed to provide £45,000 of funding which we have to match. Although we have an in kind contribution from SoftCell Biologicals of $50,000 and the student Dr Inga Williams is covering her own fees and stipend we are still £30,000 short of making the matched funding"
Full project plan and donation link at https://www.wrh.ox.ac.uk/team/karl-morten (towards bottom of page)
Action for ME have agreed to fund a new PhD student project exploring the role of the leaky gut, markers of infection and the presence of pathogenic organisms in patients with ME/CFS, Chronic Lyme Disease and Long Covid.
The project is due to start in October 2021 and will look to recruit patients in 2022.
Action for ME have agreed to provide £45,000 of funding which we have to match. Although we have an in kind contribution from SoftCell Biologicals of $50,000 and the student Dr Inga Williams is covering her own fees and stipend we are still £30,000 short of making the matched funding"
Full project plan and donation link at https://www.wrh.ox.ac.uk/team/karl-morten (towards bottom of page)
Dolphin
Senior Member (Voting Rights)
"EXCITING NEW RESEARCH INITIATIVE IN ME/CFS, CHRONIC LYME DISEASE AND LONG COVID
Action for ME have agreed to fund a new PhD student project exploring the role of the leaky gut, markers of infection and the presence of pathogenic organisms in patients with ME/CFS, Chronic Lyme Disease and Long Covid.
The project is due to start in October 2021 and will look to recruit patients in 2022.
Action for ME have agreed to provide £45,000 of funding which we have to match. Although we have an in kind contribution from SoftCell Biologicals of $50,000 and the student Dr Inga Williams is covering her own fees and stipend we are still £30,000 short of making the matched funding"
Full project plan and donation link at https://www.wrh.ox.ac.uk/team/karl-morten (towards bottom of page)
Code:
https://www.facebook.com/mortengroupoxford/posts/349284756798946Dolphin
Senior Member (Voting Rights)
Looks like someone gave £10,000, meaning they only need £3000, now.
Andy
Senior Member (Voting rights)
Twitter threads with updates from Karl's group.
Sly Saint
Senior Member (Voting Rights)
Only available to people at Oxford University but thought it worth posting
Seminar 19 October 2021, 13:00
The role of the microbiome in fatigue: does sex make a difference?
https://talks.ox.ac.uk/talks/id/e8fd95fb-d187-4ed2-b0d0-876c5bd77163/
Seminar 19 October 2021, 13:00
The role of the microbiome in fatigue: does sex make a difference?
Microbial imbalance of the intestinal biome is a key associated factor in many chronic conditions including Myalgic Encephalomyelitis (ME/CFS). Our major research goals are too increase our understanding of ME/CFS and open up new treatment options. If a leaky gut is a key component of ME/CFS, restoring a normal gut microbiome balance could be a life changing treatment options. Our collaborator SoftCell Biologicals Research (SBR) have developed approaches examining the host tissue biome. This is an un-tapped area of medicine with the presence of significant levels of wall-less (L-Form) opportunistic pathogens present in many chronic disease states. Using novel L-Form culturing methods SBR have treated L-form cultures from patients with chronic urinary tract infections (CURTIs) using a standard antibiotic panel. Clinicians acting on this information have noticed improvements in a number of patients. Clinical studies, using this approach will allow antibiotics tested in the laboratory to be used to treat patients in a blinded trial setting. In this presentation, I will highlight our research with the Doveclinic exploring levels of gut dysbiosis in a broad range of conditions many of whom suffer with fatigue. The impact of age and sex on the gut microbiome will be explored with a focus on ME/CFS and cancer. Exciting data from a comparison of recent trials of Gut Floral Replacement Therapy (GFTR) to the more conventional Faecal Microbiota transplantation (FMT) will be presented.
https://talks.ox.ac.uk/talks/id/e8fd95fb-d187-4ed2-b0d0-876c5bd77163/
Andy
Senior Member (Voting rights)
Further update.
Dolphin
Senior Member (Voting Rights)
Thread with update
Ravn
Senior Member (Voting Rights)
Not sure where to put this.
Just stumbled across this article about a researcher in Tasmania who's interested in chronic fatigue (unclear if plus or minus the syndrome bit) and who's currently learning the hard way what abnormal fatigue feels like, courtesy of Covid.
Looked up his profile and he seems to do a lot of work on brain blood flow in various diseases (ME isn't mentioned) but this bit caught my eye:
Just stumbled across this article about a researcher in Tasmania who's interested in chronic fatigue (unclear if plus or minus the syndrome bit) and who's currently learning the hard way what abnormal fatigue feels like, courtesy of Covid.
https://www.stuff.co.nz/national/he...rofessor-dont-underestimate-the-covid19-virus“It’s really interesting now because I know a lot about fatigue just from reading and the theory behind it, but now I’m experiencing it. You can actually understand how patients feel when they describe the fatigue.”
Covid-19 would now become part of his research into chronic fatigue, Sutherland said.
Looked up his profile and he seems to do a lot of work on brain blood flow in various diseases (ME isn't mentioned) but this bit caught my eye:
https://www.utas.edu.au/profiles/staff/health/brad-sutherlandInternationally, Brad continues to collaborate with Prof Alastair Buchan, A/Prof James Kennedy, A/Prof Nicola Sibson, A/Prof Gabriele De Luca and Dr Karl Morten from the University of Oxford (UK) on a range of stroke, Alzheimer’s disease and metabolism-related projects.
