A sort of quick abstract if you don't want to read it all
I looked at red blood cell count, and it was positively correlated with brain fog in ME/CFS. High RBC might be a marker of low oxygen.
I then tested all blood markers. After multiple test correction, total bilirubin (pos), relative lymphocytes (neg), and relative neutrophils (pos) are (close to) significantly correlated with brain fog.
-----------------------------
Background for why I looked at this. Skip to past dividing line to see data.
This post gave me a bit of inspiration:
Researchers from the University of Iowa in Iowa City set out to assess associations between pulmonary MRI gas exchange, structural and functional brain MRI, and cognition in long COVID patients. In pulmonary gas exchange, oxygen moves from the lungs to the bloodstream, while carbon dioxide moves from the bloodstream to the lungs.
[...]
The results showed that lower pulmonary gas exchange may be associated with cognitive dysfunction
I've noticed on my own lab tests that only one test, red blood cell count, has been consistently near or slightly above the max of the reference range, at least in the last few years.
Cleveland Clinic says the range is 4.5 to 6.1 for males, and mine have been between 5.7 and 6.5. Hematocrit and hemoglobin, less high, but still near the top of the reference range.
Not sure why it suddenly got high 3 years ago. I don't think my brain fog, or any other symptoms, significantly increased then. It could be that from 2019 to 2023, I was slowly tapering off of a medication, clozapine, which might align with the value increasing over that time. The reason I have a bajillion blood tests is because there's a risk of severely low neutrophil count with that medication, so they needed to monitor it. Now I'm off the med (and all other meds for most of the time since early 2023).
Cleveland Clinic and
Wikipedia say one of the most common causes of high red blood cell count is low oxygen. Though my oxygen saturation is usually normal, around 98%. Sleep apnea can be a cause, and I did do a sleep lab a few months ago, which showed very mild sleep apnea. I have been using CPAP for a couple months, with no change in symptoms, and RBC was still high at the most recent two tests that were after over a month of use.
Wikipedia said:
Polycythemia (also known as
polycythaemia) is a laboratory finding in which the
hematocrit (the
volume percentage of
red blood cells in the
blood) and/or
hemoglobin concentration are increased in the blood. Polycythemia is sometimes called
erythrocytosis, and there is significant overlap in the two findings, but the terms are not the same: polycythemia describes any increase in hematocrit and/or hemoglobin, while erythrocytosis describes an increase specifically in the number of red blood cells in the blood.
Secondary polycythemia is the most common cause of polycythemia. It occurs in reaction to chronically
low oxygen levels, medications, other genetic mutations that impact the body's ability to transport or detect oxygen, or, rarely because of certain cancers.
[4]
------------------------------------
So thinking RBC might be a marker of low oxygen, I was wondering if I could see a relationship between RBC and brain fog score in the NIH Deep Phenotyping data.
I looked at the "Brief Fatigue Inventory" and "Clinical Master Labs" datasets, found under "Post-Infectious MECFS at the NIH: Clinical Data Files" on mapmecfs.org.
The "Brief Fatigue Inventory" includes these items:
NIH_BFI_DIFFICULTY_CONCENTRATE
NIH_BFI_MOTIVATE_START_ACTIVITIES
NIH_BFI_FEEL_TENSE_PT
NIH_BFI_FEEL_TENSE_NURSE
NHL_BFI_FEEL_FATIGUE
NIH_BFI_DIFFICULTY_PERFORM_ACTIVITIES
NIH_BFI_HEAVINESS_LIMBS
NIH_BFI_SLOWNESS_THOUGHT_NURSE
NIH_BFI_SCORE [Combined sum of the rest of the scores]
The two that look relevant to brain fog:
NIH_BFI_DIFFICULTY_CONCENTRATE
Do you have difficulty concentrating or collecting your thoughts in the past week? 0 No Difficulty 1 2 Occasional Difficulty 3 4 Moderate Difficulty 5 6 Great Difficulty Examples of Follow-up Questions (as needed): How has your memory been this past week? Reading? Watching TV? Holding a conversation? Difficulty getting your thoughts started? How about making minor decisions? Have you been getting easily distracted?
NIH_BFI_SLOWNESS_THOUGHT_NURSE
Nurse Observation Only: slowness of thought and speech impaired ability to concentrate decreased motor activity? 0 Normal Speech And Thought 1 Some Slowness with Response 2 Obvious Slowness with Response 3 Interview Difficult 4 Complete Stupor
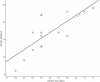
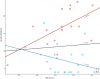
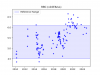
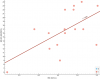
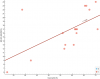
I added the two scores up into a "brain fog" score. This is for ME/CFS participants only. Looks like there might be a correlation with "RBC (M/mcL)". Pearson's r correlation is 0.46, p = 0.070.
They did another fatigue questionnaire, "Multidimensional Fatigue Inventory", which includes a "MENTAL_FATIGUE_SCALE" score that matches what I get from summing up these questions:
MFI_FOCUS_THOUGHTS: When I am doing something I can keep my thoughts on it
MFI_THOUGHTS_WANDER: My thoughts easily wander
MFI_EFFORT_CONCENTRATE: It takes a lot of effort to concentrate on things
MFI_CONCENTRATE: I can concentrate well
If I use that it's even more correlated with RBC count. r = 0.52, p = 0.032
And if I add the scores from both surveys together, it's even more correlated.
r = 0.60, p = 0.013
I also tested correlations of every blood test they have with the combined brain fog score, and did Benjamini-Hochberg correction. Let me know if you can't see the data from embedding a Google Sheet, and I'll post it another way.
"
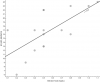
Bilirubin Total (mg/dL)" (positively correlated) and "
CD8/CD3 (#/mcL)" (negatively correlated) both have corrected p-values of 0.0604.
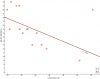
Edit: I added Spearman correlations in case some of the assumptions of Pearson are not met. Click the tab at the bottom of the spreadsheet above to switch to Spearman. Bilirubin still in the top spot, but now
Lymphocytes (%) are negatively correlated and
Neutrophil (%) positively correlated with brain fog with corrected p-values of 0.063.
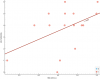
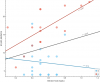
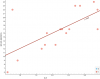
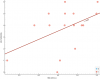
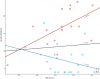
Edit2: Plotted bilirubin to see what's so special. It does look like a strong correlation with brain fog.
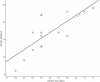
Note: One participant was excluded for the bilirubin calculation because their lab value is "<0.2", which is not a specific number. Their brain fog score is 17. If I guess and say their bilirubin is 0.1 so that they are included, then it does decrease the correlation a bit:
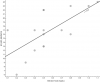
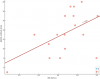
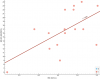
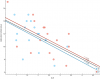
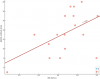
Edit3: And here are lymphocytes and neutrophils:
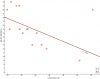
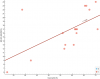
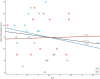
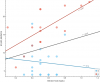
Edit4: If including healthy participants, the correlation goes down for all the ones I plotted. For example, RBC and bilirubin (blue is healthy):
Edit5: And just a note about the MFI questionnaire, since I just noticed and was confused by why it seems to ask for a 1 to 5 score for opposite statements like "It takes a lot of effort to concentrate on things" and "I can concentrate well" and then adds them up. I found
instructions for the MFI-20 which say the positively worded questions have to be reversed (so 5 becomes 1, etc). It seems they have done that with the mapmecfs data so the scores can be safely added.