John Mac
Senior Member (Voting Rights)
Abstract
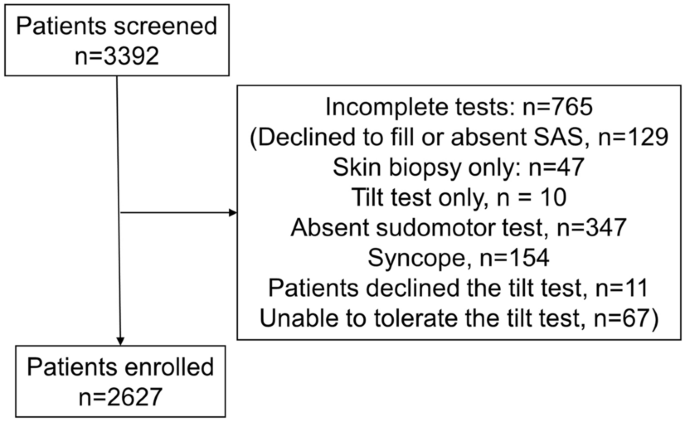
Background/Objectives: Symptoms of autonomic dysfunction are common in infection-associated chronic conditions and illnesses (IACCIs), including myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS). This study aimed to evaluate autonomic symptoms and their impact on ME/CFS illness severity.Methods: Data came from a multi-site study conducted in seven ME/CFS specialty clinics during 2012–2020. Autonomic dysfunction was assessed using the Composite Autonomic Symptom Scale 31 (COMPASS-31), medical history, and a lean test originally described by the National Aeronautics and Space Administration (NASA). Illness severity was assessed using Patient-Reported Outcomes Measurement Information System measures, the 36-item short-form, as well as the CDC Symptom Inventory. This analysis included 442 participants who completed the baseline COMPASS-31 assessment, comprising 301 individuals with ME/CFS and 141 healthy controls (HC).
Results: ME/CFS participants reported higher autonomic symptom burden than HC across three assessment tools (all p < 0.0001), including the COMPASS-31 total score (34.1 vs. 6.8) and medical history indicators [dizziness or vertigo (42.6% vs. 2.8%), cold extremities (38.6% vs. 5.7%), and orthostatic intolerance (OI, 33.9% vs. 0.7%)]. Among ME/CFS participants, 97% had at least one autonomic symptom. Those with symptoms in the OI, gastrointestinal, and pupillomotor domains had significantly higher illness severity than those without these symptoms.
Conclusions: ME/CFS patients exhibit a substantial autonomic symptom burden that correlates with greater illness severity. Individualized care strategies targeting dysautonomia assessment and intervention may offer meaningful improvements in symptom management and quality of life for those with ME/CFS and similar chronic conditions.