The therapies tested under the PACE trial are based on two overlapping psychological models for CFS: fear avoidance and deconditioning. We believe that the blanket application of this psychological profile to patients satisfying the Oxford criteria has been conclusively dismissed by the weak results of the PACE trial. It is our belief that it is only the persistent use of the Oxford criteria that has allowed the survival of this model, which is dependent on a mix of very different conditions to produce a variable and generally weak outcome.
The two principal therapies used, Graded Exercise and Cognitive Behaviour Therapies, should have been very effective on these psychological profiles, so the failure to deliver such an effect utterly negates the blanket assumption. However, it is clear that some patients showed distinct improvement under these therapies, so within the vast amount of data gathered, there must be information that allows us to determine why that is so. However, there is simply far too much data for just one team to analyse. The data must be made available for a number of different approaches and perceptions to be applied to it.
We believe that the results can be explained through a different model, and offer it as an example. Obviously we do not have access to the raw data, so this is purely speculative, based on the parameters set out by the PACE study. It was very difficult in our model to simultaneously match both the low mean/average improvements in the PACE trial, and the relatively large standard deviation quoted, while still keeping in line with the numbers that improved by 2 or more points and the numbers that reached 18 points or fewer with the findings implied in the PACE trial. This suggests that the contrasts between the three subgroups is greater than in this model, and that the average change may have been driven by a smaller number doing proportionately better. This model is just a first approximation. Click here if you would like to download the Excel file and investigate further.
Our model splits those patients selected through the Oxford criteria into three roughly equal groups, with the third being slightly larger than the other two.
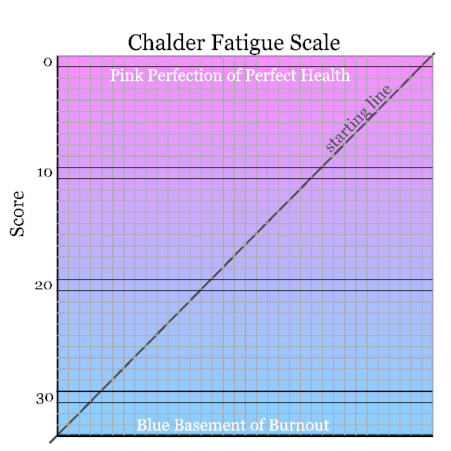
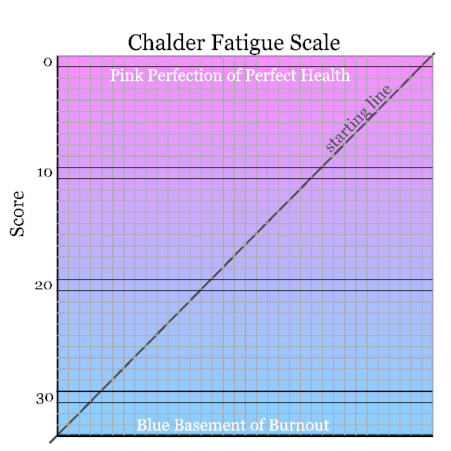
The first group has entirely biomedical needs. Their symptoms can be improved through effective pain control and help with sleep patterns, such as was offered as part of the Specialist Medical Care that all groups received. It is likely that the greatest improvements would be seen by those who have had the illness for the least amount of time, as they have had less time to discover effective pain and sleep treatments. Their Chalder Fatigue scores on the continuous/Likert scale range is a uniform random distribution from 21 to 33 points.
The second group is essentially the same as the first group, with a similar range of underlying biomedical needs. But in addition to that, they have further factors adding to their difficulties (adding between 4 to 10 points to their score). These are along the lines of worry about the true nature of what is wrong with them (covered in 4-more), and of doing too much during good patches due to a lack of experience in coping with the illness. Another part of the additional component would be simply caused by the stress of starting something new in unfamiliar surroundings.
Because this component is added to the biological component of the members of the first group, it worsens their fatigue and increases their fatigue scores, causing a clumping effect around the worst possible scores. Note that improving the additional component could easily mask any ill-effects on the biological component.
Patients in this second group are likely to have had the illness for less than the average time, and less likely to be members of a support group (where they would have gained better knowledge of the illness, and of the consequences of overexertion).
The third group has problems that have a substantial psychological component, although a precipitating biomedical cause cannot be ruled out. We are not in a position to offer any comments as to the nature of that psychological component, but as it is improved as much by Specialist Medical Care as by many more additional sessions of therapy, we do not feel that the underlying PACE psychological assumption is particularly appropriate. (It has been shown by Ridsdale et al. that counselling can be as effective as CBT.) Their Chalder Fatigue scores on the continuous/Likert scale range is also a uniform random distribution from 21 to 33 points. It is the use of the Oxford criteria that permits this group to be so large, but it must not be assumed that the "international criteria" excludes these patients.
Patients who would satisfy the Canadian criteria for ME, would fall into the first two groups, but there will be other biomedical conditions in those groups as well – some simply undiagnosed but with a recognised condition, others with a unknown biomedical condition.
The diagrams below simulate the recovery patterns for these theoretical patients. The overall pattern matches the parameters given in the report on the PACE trial, so although the whole exercise is theoretical, we believe that it will be a moderate match of the true results, although, without the real-life fluctuations, ours suffers from "clumping" in places. Click on each numbered button to see the appropriate diagram.
|