Dolphin
Senior Member (Voting Rights)
The Role of Neuroinflammation in Post-Exertional Malaise Among Chronic Multisymptom Illness
By Jacob V. Ninneman
A dissertation submitted in partial fulfillment of the requirements for the degree of Doctor of Philosophy (Kinesiology) At the UNIVERSITY OF WISCONSIN-MADISON 2025
Date of final oral examination: 08/14/2025
This dissertation is approved by the following members of the Final Oral Committee:
Dane B. Cook, Professor, Kinesiology
Bradley T. Christian, Professor, Medical Physics
Jacob Meyer, Professor, Kinesiology
Doug Dean III, Professor, Pediatrics
Daniel Bolt, Professor, Education Psychology
Abstract ii
Introduction:
Chronic Multisymptom Illnesses (CMIs) (e.g., Long COVID, Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS), and Gulf War Illness (GWI)) are characterized by chronic fatigue, pain, and neurocognitive complaints without a clear underlying pathology. Instead of experiencing the salubrious response typically associated with exercise, those with CMI experience a worsening of symptoms post-exercise, termed post-exertional malaise (PEM). Physiology at rest has not adequately explained CMI symptoms; therefore experimental models of PEM are used to better understand both disease pathophysiology and symptom worsening. The limited evidence available suggests that exercise can stimulate peripheral inflammation in CMI, although the data are mixed. It is unknown whether exercise induce central nervous system inflammation (i.e. neuroinflammation).
Purpose:
To investigate neuroinflammation at rest and in response to an acute exercise challenge in CMI.
Methods:
14 CMI (6 Long COVID, 6 ME/CFS, and 2 GWI) and 14 age and sex matched controls (CON) were recruited. Inclusion criteria consisted of meeting the World Health Organization criteria for Long COVID, the Canadian Consensus Criteria for ME/CFS, and the Kansas Case definition for GWI. Positron emission tomography (PET) imaging and symptom measurement, took place one week prior to and 24 hours following a standardized exercise test. Additionally, symptoms measurement occurred for one week post exercise. PET imaging consisted of a 70 minute dynamic scan with a third generation translocator protein radiotracer – 11C-ER176. Exercise consisted of 30 minutes of moderate intensity cycling (70% Heart Rate Reserve) with continuous collection of the cardiometabolic response with a Parvo metabolic cart. All PET images were normalized to a standardized space and corrected for the injected dose and whole brain binding. Groups were compared at baseline and post-exercise with an analysis of covariance (ANCOVA) controlling for genotype or genotype and age and sex. A repeated measures ANCOVA controlling for either genotype or genotype, age, and sex was used to compare the response to exercise between CMI and CON. Relationships with symptoms were tested with multiple linear regressions.
Results:
As expected, CMI reported worse fatigue, pain, mental and physical functioning, sleep, mood, as well as lower levels of physical activity relative to CON. CMI and CON were able to maintain their prescribed intensity for a similar percentage of the test (CMI: 83.5%, CON: 90.1, p = 0.17). Cardiometabolic and perceptual responses were similar with only average fatigue being significantly different between groups. Significant group x time interactions were identified for fatigue (F(2,81) = 6.38, p = 0.003), pain (F(2,81) =6.06, p = 0.004), and neurocognitive symptoms (F(2,81) =9.8, p < 0.001). Neuroinflammation was significantly higher in CMI compared CON both pre- and post-exercise; and occurred diffusely across the brain. No specific brain regions were differentially impacted by exercise in either CMI nor CON with small effect size differences for all regions tested.
Conclusions:
Long COVID report similar impacts on their health and functioning, as well as a similar PEM experience as ME/CFS when tested experimentally. Widespread neuroinflammation is present in CMI, but does not appear to be affected 24 hours post-exercise. Future studies should incorporate both peripheral and central measures of inflammation to evaluate potential exaggeration of peripheral immune responses and their correlation with central nervous system inflammation. Larger cohorts with broader ranges of illness severity and duration are essential to generalizability.
By Jacob V. Ninneman
A dissertation submitted in partial fulfillment of the requirements for the degree of Doctor of Philosophy (Kinesiology) At the UNIVERSITY OF WISCONSIN-MADISON 2025
Date of final oral examination: 08/14/2025
This dissertation is approved by the following members of the Final Oral Committee:
Dane B. Cook, Professor, Kinesiology
Bradley T. Christian, Professor, Medical Physics
Jacob Meyer, Professor, Kinesiology
Doug Dean III, Professor, Pediatrics
Daniel Bolt, Professor, Education Psychology
Abstract ii
Introduction:
Chronic Multisymptom Illnesses (CMIs) (e.g., Long COVID, Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS), and Gulf War Illness (GWI)) are characterized by chronic fatigue, pain, and neurocognitive complaints without a clear underlying pathology. Instead of experiencing the salubrious response typically associated with exercise, those with CMI experience a worsening of symptoms post-exercise, termed post-exertional malaise (PEM). Physiology at rest has not adequately explained CMI symptoms; therefore experimental models of PEM are used to better understand both disease pathophysiology and symptom worsening. The limited evidence available suggests that exercise can stimulate peripheral inflammation in CMI, although the data are mixed. It is unknown whether exercise induce central nervous system inflammation (i.e. neuroinflammation).
Purpose:
To investigate neuroinflammation at rest and in response to an acute exercise challenge in CMI.
Methods:
14 CMI (6 Long COVID, 6 ME/CFS, and 2 GWI) and 14 age and sex matched controls (CON) were recruited. Inclusion criteria consisted of meeting the World Health Organization criteria for Long COVID, the Canadian Consensus Criteria for ME/CFS, and the Kansas Case definition for GWI. Positron emission tomography (PET) imaging and symptom measurement, took place one week prior to and 24 hours following a standardized exercise test. Additionally, symptoms measurement occurred for one week post exercise. PET imaging consisted of a 70 minute dynamic scan with a third generation translocator protein radiotracer – 11C-ER176. Exercise consisted of 30 minutes of moderate intensity cycling (70% Heart Rate Reserve) with continuous collection of the cardiometabolic response with a Parvo metabolic cart. All PET images were normalized to a standardized space and corrected for the injected dose and whole brain binding. Groups were compared at baseline and post-exercise with an analysis of covariance (ANCOVA) controlling for genotype or genotype and age and sex. A repeated measures ANCOVA controlling for either genotype or genotype, age, and sex was used to compare the response to exercise between CMI and CON. Relationships with symptoms were tested with multiple linear regressions.
Results:
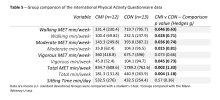
As expected, CMI reported worse fatigue, pain, mental and physical functioning, sleep, mood, as well as lower levels of physical activity relative to CON. CMI and CON were able to maintain their prescribed intensity for a similar percentage of the test (CMI: 83.5%, CON: 90.1, p = 0.17). Cardiometabolic and perceptual responses were similar with only average fatigue being significantly different between groups. Significant group x time interactions were identified for fatigue (F(2,81) = 6.38, p = 0.003), pain (F(2,81) =6.06, p = 0.004), and neurocognitive symptoms (F(2,81) =9.8, p < 0.001). Neuroinflammation was significantly higher in CMI compared CON both pre- and post-exercise; and occurred diffusely across the brain. No specific brain regions were differentially impacted by exercise in either CMI nor CON with small effect size differences for all regions tested.
Conclusions:
Long COVID report similar impacts on their health and functioning, as well as a similar PEM experience as ME/CFS when tested experimentally. Widespread neuroinflammation is present in CMI, but does not appear to be affected 24 hours post-exercise. Future studies should incorporate both peripheral and central measures of inflammation to evaluate potential exaggeration of peripheral immune responses and their correlation with central nervous system inflammation. Larger cohorts with broader ranges of illness severity and duration are essential to generalizability.