Proteomic analysis of post-COVID condition: Insights from plasma and pellet blood fractions
Alejandro Seco-González, Paula Antelo-Riveiro, Susana B. Bravo, P.F. Garrido, M.J. Domínguez-Santalla, E. Rodríguez-Ruiz, Á. Piñeiro, R. Garcia-Fandino
Background
Persistent symptoms extending beyond the acute phase of SARS-CoV-2 infection, known as Post-COVID condition (PCC), continue to impact many individuals years after the COVID-19 pandemic began. This highlights an urgent need for a deeper understanding and effective treatments. While significant progress has been made in understanding the acute phase of COVID-19 through omics-based approaches, the proteomic alterations linked to the long-term effects of the infection remain underexplored. This study aims to investigate these proteomic changes and develop a method for stratifying disease severity.
Methods
Using Sequential Window Acquisition of All Theoretical Fragment Ion Mass Spectra (SWATH-MS) technology, we performed comprehensive proteomic profiling of blood samples from 65 PCC patients. Both plasma and pellet (cellular components) fractions were analyzed to capture a wide array of proteomic changes associated with PCC.
Results
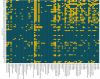
Proteomic profiling revealed distinct differences between symptomatic and asymptomatic PCC patients. In the plasma fraction, symptomatic patients exhibited significant upregulation of proteins involved in coagulation, immune response, oxidative stress, and various metabolic processes, while certain immunoglobulins and proteins involved in cellular stress responses were downregulated. In the pellet fraction, symptomatic patients showed upregulation of proteins related to immune response, coagulation, oxidative stress, and metabolic enzymes, with downregulation observed in components of the complement system, glycolysis enzymes, and cytoskeletal proteins. A key outcome was the development of a novel severity scale based on the concentration of identified proteins, which correlated strongly with the clinical symptoms of PCC. This scale, derived from unsupervised clustering analysis, provides precise quantification of PCC severity, enabling effective patient stratification.
Conclusions
The identified proteomic alterations offer valuable insights into the molecular mechanisms underlying PCC, highlighting potential biomarkers and therapeutic targets. This research supports the development of tailored clinical interventions to alleviate persistent symptoms, ultimately enhancing patient outcomes and quality of life. The quantifiable measure of disease severity aids clinicians in understanding the condition in individual patients, facilitating personalized treatment plans and accurate monitoring of disease progression and response to therapy.
Link | PDF (Journal of Infection and Public Health) [Open Access]
Alejandro Seco-González, Paula Antelo-Riveiro, Susana B. Bravo, P.F. Garrido, M.J. Domínguez-Santalla, E. Rodríguez-Ruiz, Á. Piñeiro, R. Garcia-Fandino
Background
Persistent symptoms extending beyond the acute phase of SARS-CoV-2 infection, known as Post-COVID condition (PCC), continue to impact many individuals years after the COVID-19 pandemic began. This highlights an urgent need for a deeper understanding and effective treatments. While significant progress has been made in understanding the acute phase of COVID-19 through omics-based approaches, the proteomic alterations linked to the long-term effects of the infection remain underexplored. This study aims to investigate these proteomic changes and develop a method for stratifying disease severity.
Methods
Using Sequential Window Acquisition of All Theoretical Fragment Ion Mass Spectra (SWATH-MS) technology, we performed comprehensive proteomic profiling of blood samples from 65 PCC patients. Both plasma and pellet (cellular components) fractions were analyzed to capture a wide array of proteomic changes associated with PCC.
Results
Proteomic profiling revealed distinct differences between symptomatic and asymptomatic PCC patients. In the plasma fraction, symptomatic patients exhibited significant upregulation of proteins involved in coagulation, immune response, oxidative stress, and various metabolic processes, while certain immunoglobulins and proteins involved in cellular stress responses were downregulated. In the pellet fraction, symptomatic patients showed upregulation of proteins related to immune response, coagulation, oxidative stress, and metabolic enzymes, with downregulation observed in components of the complement system, glycolysis enzymes, and cytoskeletal proteins. A key outcome was the development of a novel severity scale based on the concentration of identified proteins, which correlated strongly with the clinical symptoms of PCC. This scale, derived from unsupervised clustering analysis, provides precise quantification of PCC severity, enabling effective patient stratification.
Conclusions
The identified proteomic alterations offer valuable insights into the molecular mechanisms underlying PCC, highlighting potential biomarkers and therapeutic targets. This research supports the development of tailored clinical interventions to alleviate persistent symptoms, ultimately enhancing patient outcomes and quality of life. The quantifiable measure of disease severity aids clinicians in understanding the condition in individual patients, facilitating personalized treatment plans and accurate monitoring of disease progression and response to therapy.
Link | PDF (Journal of Infection and Public Health) [Open Access]