Practical Recommendations for Exercise Training in Patients with Long COVID with or without Post-exertional Malaise: A Best Practice Proposal
Gloeckl, Rainer; Zwick, Ralf H.; Fürlinger, Ulrich; Schneeberger, Tessa; Leitl, Daniela; Jarosch, Inga; Behrends, Uta; Scheibenbogen, Carmen; Koczulla, Andreas Rembert
People with long COVID may suffer from a wide range of ongoing symptoms including fatigue, exertional dyspnea, reduced exercise performance, and others. In particular, impaired exercise performance is a condition that can be recovered in many people through an individualized physical exercise training program. However, clinical experience has shown that the presence of post-exertional malaise (PEM) is a significant barrier to physical exercise training in people with long COVID. Currently, there is no guideline or consensus available on how to apply exercise training in this cohort.
Therefore, we conducted a literature review in the PubMed library using the following search terms: “COVID”, “post-COVID”, “long COVID” and “exercise” searching for studies from January 2020 to January 2024. Data from 46 trials were included. Exercise training regimes were very heterogeneous and none of these studies reported on the management of PEM in the context of an exercise training program. Based on the feedback from an additional survey that was answered by 14 international experts in the field of exercise training in long COVID, combined with the authors´ own extensive practical experience, a best practice proposal for exercise training recommendations has been developed.
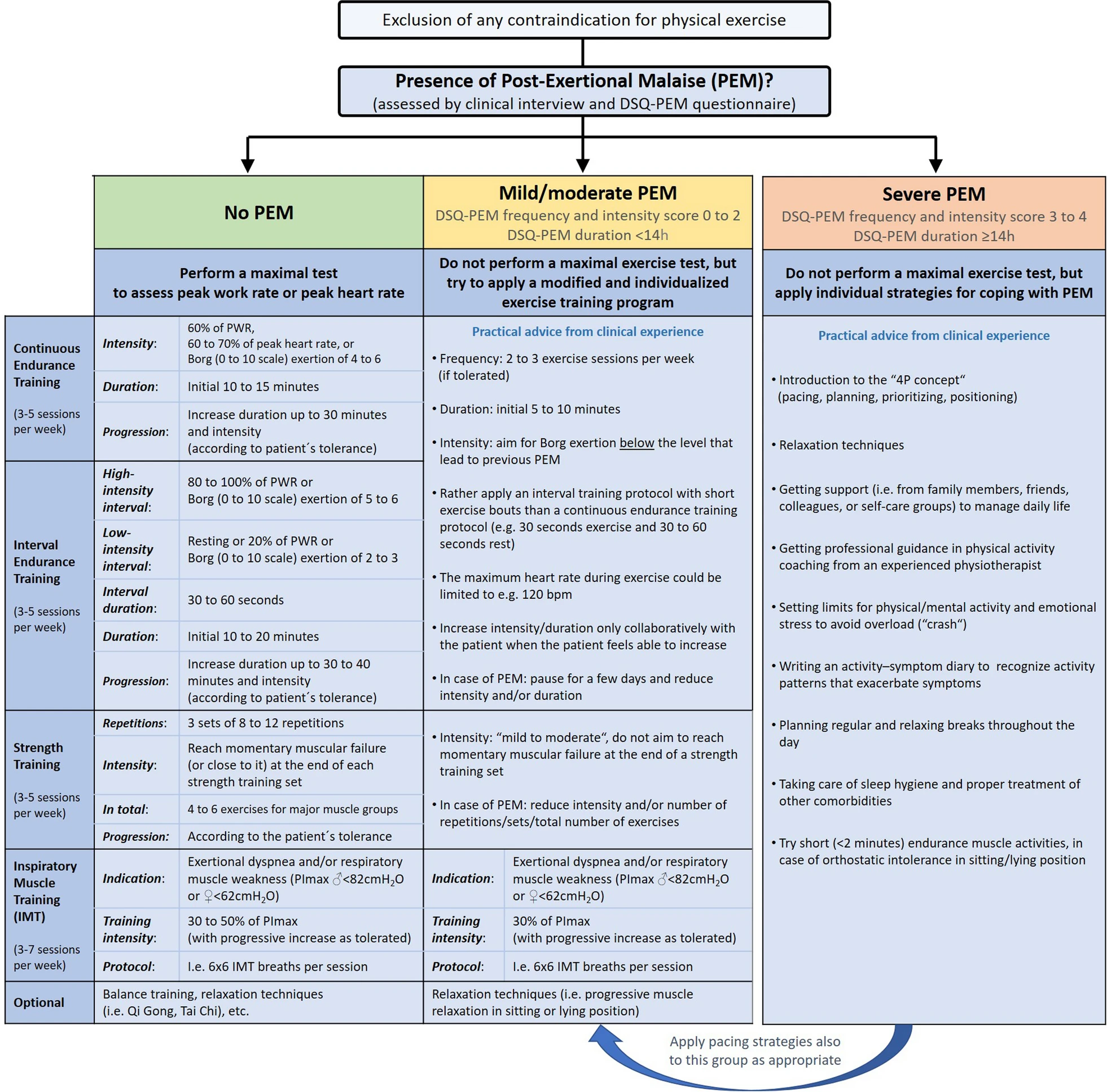
This proposal differentiates exercise procedures according to the presence of no, mild/moderate or severe PEM in people with long COVID. These recommendations may guide allied healthcare professionals worldwide in initiating and adjusting exercise training programs for people with long COVID, stratified according to the presence and severity of PEM.
Link | PDF (Sports Medicine - Open) [Open Access]
Gloeckl, Rainer; Zwick, Ralf H.; Fürlinger, Ulrich; Schneeberger, Tessa; Leitl, Daniela; Jarosch, Inga; Behrends, Uta; Scheibenbogen, Carmen; Koczulla, Andreas Rembert
People with long COVID may suffer from a wide range of ongoing symptoms including fatigue, exertional dyspnea, reduced exercise performance, and others. In particular, impaired exercise performance is a condition that can be recovered in many people through an individualized physical exercise training program. However, clinical experience has shown that the presence of post-exertional malaise (PEM) is a significant barrier to physical exercise training in people with long COVID. Currently, there is no guideline or consensus available on how to apply exercise training in this cohort.
Therefore, we conducted a literature review in the PubMed library using the following search terms: “COVID”, “post-COVID”, “long COVID” and “exercise” searching for studies from January 2020 to January 2024. Data from 46 trials were included. Exercise training regimes were very heterogeneous and none of these studies reported on the management of PEM in the context of an exercise training program. Based on the feedback from an additional survey that was answered by 14 international experts in the field of exercise training in long COVID, combined with the authors´ own extensive practical experience, a best practice proposal for exercise training recommendations has been developed.
This proposal differentiates exercise procedures according to the presence of no, mild/moderate or severe PEM in people with long COVID. These recommendations may guide allied healthcare professionals worldwide in initiating and adjusting exercise training programs for people with long COVID, stratified according to the presence and severity of PEM.
Link | PDF (Sports Medicine - Open) [Open Access]