V.R.T.
Senior Member (Voting Rights)
Just to add to this, I did a bit of research the other day to refresh my memory. The questionaire was the COMPASS-31.An IgG degrader called efgartigimod (vvygart) was trialed in long covid a couple of years back. It was trialled for POTS, and the primary outcome was a questionaire called COMPASS or something similar.
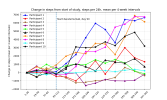
Many people in the trial reported significant improvement in PEM and POTS/OI, including improved readings on tilt table tests. The drug company ignored all of this, and because it wasnt picked up on their questionnaire, declared the trial failed.
The patients say the questionnaire was a terrible measure of improvement, and last I heard were campaigning for the release of the raw data. I don't think the study tracked PEM at all.
As we have discussed elsewhere in regard to other drugs we can't say for sure why these people improved but a mechanism like you propose here could probably explain it.
And there were participants on reddit and in a private lc group im a member of saying they went from having heart rates shoot up from 60ish to 160 on tilt tests to not being symptomatic during a tilt, and not meeting pots criterea anymore. The tilts were part of the trial so i have no idea why this was ignored. Improved PEM was also reported as I said.