Persistent endothelial dysfunction in post-COVID-19 syndrome and its associations with symptom severity and chronic inflammation
Timon Kuchler; Roman Günthner; Andrea Ribeiro; Renate Hausinger; Lukas Streese; Anna Wöhnl; Veronika Kesseler; Johanna Negele; Tarek Assali; Javier Carbajo-Lozoya; Maciej Lech; Kristina Adorjan; Hans Christian Stubbe; Henner Hanssen; Konstantin Kotilar; Berhard Haller; Uwe Heemann; Christoph Schmaderer
Background
Post-COVID-19 syndrome (PCS) is a lingering disease with ongoing symptoms such as fatigue and cognitive impairment resulting in a high impact on the daily life of patients. Understanding the pathophysiology of PCS is a public health priority, as it still poses a diagnostic and treatment challenge for physicians.
Methods
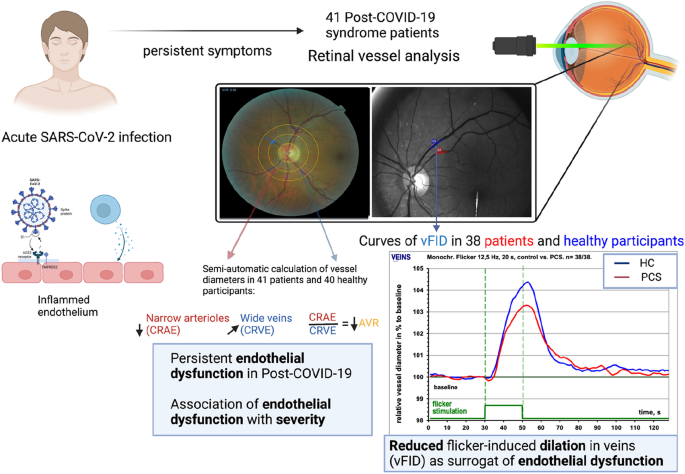
In this prospective observational cohort study, we analyzed the retinal microcirculation using Retinal Vessel Analysis (RVA) in a cohort of patients with PCS and compared it to an age- and gender-matched healthy cohort (n=41, matched out of n = 204).
Measurements and main results
PCS patients exhibit persistent endothelial dysfunction (ED), as indicated by significantly lower venular §icker-induced dilation (vmax; 3.42% ± 1.77% vs. 4.64 % ± 2.59%; p = 0.02), narrower central retinal artery equivalent (CRAE; 178.1 [167.5 - 190.2] vs. 189.1 [179.4 - 197.2], p = 0.01) and lower arteriolar-venular ratio (AVR; (0.84 [0.8 - 0.9] vs. 0.88 [0.8 - 0.9], p = 0.007). When combining AVR and vmax, predicted scores reached good ability to discriminate groups (area under the curve: 0.75). Higher PCS severity scores correlated with lower AVR (R= -0.37 p = 0.017). The association of microvascular changes with PCS severity were amplified in PCS patients exhibiting higher levels of in§ammatory parameters.
Conclusion
Our results demonstrate that prolonged endothelial dysfunction is a hallmark of PCS, and impairments of the microcirculation seem to explain ongoing symptoms in patients. As potential therapies for PCS emerge, RVA parameters may become relevant as clinical biomarkers for diagnosis and therapy management.
Trial Registration
This study was previously registered at ClinicalTrials (“All Eyes on PCS - Analysis of the Retinal Microvasculature in Patients With Post-COVID-19 Syndrome”. NCT05635552. https://clinicaltrials.gov/ct2/show/NCT05635552).
Link | PDF (Preprint: Research Square)
Timon Kuchler; Roman Günthner; Andrea Ribeiro; Renate Hausinger; Lukas Streese; Anna Wöhnl; Veronika Kesseler; Johanna Negele; Tarek Assali; Javier Carbajo-Lozoya; Maciej Lech; Kristina Adorjan; Hans Christian Stubbe; Henner Hanssen; Konstantin Kotilar; Berhard Haller; Uwe Heemann; Christoph Schmaderer
Background
Post-COVID-19 syndrome (PCS) is a lingering disease with ongoing symptoms such as fatigue and cognitive impairment resulting in a high impact on the daily life of patients. Understanding the pathophysiology of PCS is a public health priority, as it still poses a diagnostic and treatment challenge for physicians.
Methods
In this prospective observational cohort study, we analyzed the retinal microcirculation using Retinal Vessel Analysis (RVA) in a cohort of patients with PCS and compared it to an age- and gender-matched healthy cohort (n=41, matched out of n = 204).
Measurements and main results
PCS patients exhibit persistent endothelial dysfunction (ED), as indicated by significantly lower venular §icker-induced dilation (vmax; 3.42% ± 1.77% vs. 4.64 % ± 2.59%; p = 0.02), narrower central retinal artery equivalent (CRAE; 178.1 [167.5 - 190.2] vs. 189.1 [179.4 - 197.2], p = 0.01) and lower arteriolar-venular ratio (AVR; (0.84 [0.8 - 0.9] vs. 0.88 [0.8 - 0.9], p = 0.007). When combining AVR and vmax, predicted scores reached good ability to discriminate groups (area under the curve: 0.75). Higher PCS severity scores correlated with lower AVR (R= -0.37 p = 0.017). The association of microvascular changes with PCS severity were amplified in PCS patients exhibiting higher levels of in§ammatory parameters.
Conclusion
Our results demonstrate that prolonged endothelial dysfunction is a hallmark of PCS, and impairments of the microcirculation seem to explain ongoing symptoms in patients. As potential therapies for PCS emerge, RVA parameters may become relevant as clinical biomarkers for diagnosis and therapy management.
Trial Registration
This study was previously registered at ClinicalTrials (“All Eyes on PCS - Analysis of the Retinal Microvasculature in Patients With Post-COVID-19 Syndrome”. NCT05635552. https://clinicaltrials.gov/ct2/show/NCT05635552).
Link | PDF (Preprint: Research Square)