Optimising and beta-testing a user-centred, accessible, self-management rehabilitation smartphone app reCOVer for long-COVID fatigue using qualitative interview methods
PURPOSE
Fatigue is one of the most common and disabling symptoms of long-COVID, yet individuals often struggle to access appropriate services and must self-manage. This study aimed to adapt an existing smartphone app, originally developed for fatigue in autoimmune rheumatic disease, for individuals with long-COVID.
MATERIALS AND METHODS
A multidisciplinary steering group reviewed current clinical and scientific evidence to inform the adaptation of the app, reCOVer. The app includes an activity pacing diary, goal-setting tool, assertiveness and communication cards, and guidance on fatigue, sleep, relaxation, and setbacks. Beta-testing was conducted with 11 individuals with long-COVID (aged 21–57). Each participant took part in two serial qualitative interviews: the first explored their experience of fatigue and initial reactions to the app; the second, after 7–10 days of use, captured usability and acceptability feedback.
RESULTS
Participants found reCOVer helpful, particularly for increasing awareness of unhelpful patterns (e.g., boom–bust cycles) and supporting behaviour change through pacing. Communication tools were valuable when cognitive difficulties were prominent. Suggested improvements included text-to-speech functionality, clearer goal-setting instructions, and better articulation of app benefits.
CONCLUSIONS
reCOVer shows promise as a self-management tool for long-COVID fatigue. Further research, such as a pilot RCT, is needed to evaluate feasibility and effectiveness.
IMPLICATIONS FOR REHABILITATION
Fatigue is a debilitating symptom of long-COVID and can significantly affect daily functioning and quality of life.
Smartphone-based self-management interventions, like the reCOVer app, may offer accessible and acceptable support for individuals managing long-COVID fatigue at home.
Features such as activity diaries, pacing tools, and communication strategies can help users recognise and adapt unhelpful behaviours (e.g., boom-bust cycles), supporting behaviour change over time.
Rehabilitation professionals may consider recommending or co-developing digital tools to extend support for individuals with long-COVID, particularly in contexts where professional support is limited.
Web | PDF | Disability and Rehabilitation | Open Access
J L McCready; M Campbell; K McCay; J Moore; V Deary; J Vines; C Higgs-McCallum; D Webster; J Ellis; J Newton; C Nobbs; T Rapley; K L Hackett
PURPOSE
Fatigue is one of the most common and disabling symptoms of long-COVID, yet individuals often struggle to access appropriate services and must self-manage. This study aimed to adapt an existing smartphone app, originally developed for fatigue in autoimmune rheumatic disease, for individuals with long-COVID.
MATERIALS AND METHODS
A multidisciplinary steering group reviewed current clinical and scientific evidence to inform the adaptation of the app, reCOVer. The app includes an activity pacing diary, goal-setting tool, assertiveness and communication cards, and guidance on fatigue, sleep, relaxation, and setbacks. Beta-testing was conducted with 11 individuals with long-COVID (aged 21–57). Each participant took part in two serial qualitative interviews: the first explored their experience of fatigue and initial reactions to the app; the second, after 7–10 days of use, captured usability and acceptability feedback.
RESULTS
Participants found reCOVer helpful, particularly for increasing awareness of unhelpful patterns (e.g., boom–bust cycles) and supporting behaviour change through pacing. Communication tools were valuable when cognitive difficulties were prominent. Suggested improvements included text-to-speech functionality, clearer goal-setting instructions, and better articulation of app benefits.
CONCLUSIONS
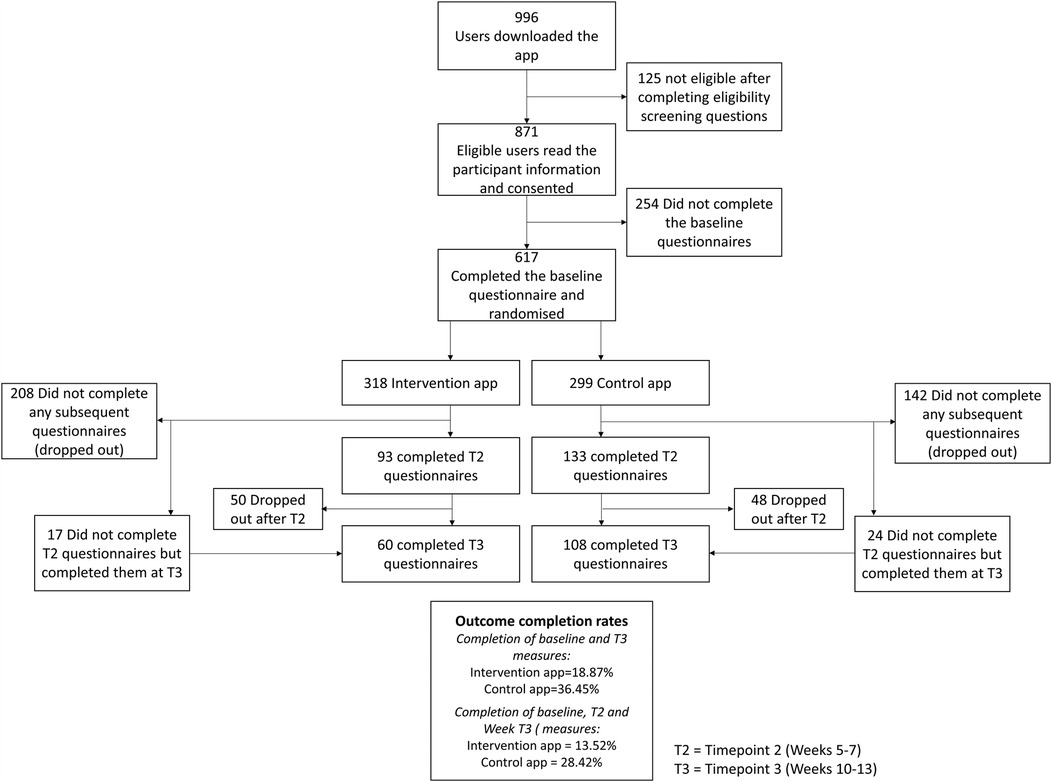
reCOVer shows promise as a self-management tool for long-COVID fatigue. Further research, such as a pilot RCT, is needed to evaluate feasibility and effectiveness.
IMPLICATIONS FOR REHABILITATION
Fatigue is a debilitating symptom of long-COVID and can significantly affect daily functioning and quality of life.
Smartphone-based self-management interventions, like the reCOVer app, may offer accessible and acceptable support for individuals managing long-COVID fatigue at home.
Features such as activity diaries, pacing tools, and communication strategies can help users recognise and adapt unhelpful behaviours (e.g., boom-bust cycles), supporting behaviour change over time.
Rehabilitation professionals may consider recommending or co-developing digital tools to extend support for individuals with long-COVID, particularly in contexts where professional support is limited.
Web | PDF | Disability and Rehabilitation | Open Access